How a Public Health Campaign in the Warsaw Ghetto Stemmed the Spread of Typhus
A new study shows how life-saving efforts by Jewish doctors helped curb an epidemic during World War II
:focal(748x360:749x361)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/9e/1e/9e1e54d3-b9c7-4738-aff1-0a1e02d818e7/gettyimages-56462756_forweb.jpg)
The Warsaw Ghetto was a horrific part of the Nazi Germany campaign to exterminate the Jewish population of Europe. As millions were killed by the SS in death camps like Auschwitz, the Jews in Poland’s capital city were held captive by the German army and subjected to starvation, forced labor and disease.
To combat the spread of illness, a new study suggests, Jews within the Ghetto may have had success in using community containment efforts not unlike the social distancing efforts recommended today in the struggle against COVID-19. The historical record shows that an epidemic of typhus, a deadly but preventable bacterial disease, ravaged the imprisoned population, but then, somehow, cases dropped dramatically.
While historians have long understood this to be the case, a new mathematical modeling study, published last week in Science Advances, brings together information from across a spectrum of sources including daily journals, government rationing records, reported case numbers and biostatics, and posits that a vibrant public health campaign was at the root of the efforts to curb the spread.
In the fall of 1940, the occupying Germany army blockaded the Polish city of Warsaw, sealing the city’s more than 400,000 Jews into a 1.3 square mile area. (For comparison, the population density of New York City is about 27,000 people per square mile.) The Germans excused and codified the containment under the guise of isolating disease-carrying individuals; Polish Jews were depicted in Nazi propaganda posters as lice, or typhus vectors.
“It's eye-opening to realize how the question of epidemics informed various decisions, including the German decision to create ghettos, and paved the way to genocide,” says Holocaust historian Tomasz Frydel, who was not involved with the study.
German officials knew enough about the spread of typhus to know that by overcrowding, starving and depriving the Jewish residents of basic necessities, the ghetto would become a breeding ground for infection. Additional food supplies were blocked until May 1941, at which point rations provided by authorities amounted to no more than 200 calories per day, per person. The starvation made fighting any disease that did emerge near impossible, and louse vectors spread easily due to a lack of adequate sanitation and an abundance of hosts.
More than 100,000 Jews were infected by typhus and at least 25,000 died directly from it. But, just before the winter of 1941, as an epidemic in the ghetto was breaking out, something remarkable happened: cases dropped exponentially when they should have continued to rise.
“My greatest surprise was realizing that the typhus epidemic died out at the very beginning of winter just when I would have expected it to accelerate,” says study author Lewi Stone, a mathematician and disease modeler with RMIT in Australia and Tel Aviv University in Israel. “For a year I thought this was likely just a corrupted dataset. But then I checked with the diary of [famed ghetto historian Emanuel] Ringelblum, who documented daily events in the ghetto, and he himself corroborated what I had seen.”
Ringelblum wrote in his diary that cases fell by 40 percent. Stone and his team set off to quantify what happened between the time the ghetto was sealed off in November 1940, until July 1942, when it was liquidated and more than 250,000 remaining Jews were sent to the Treblinka death camp.
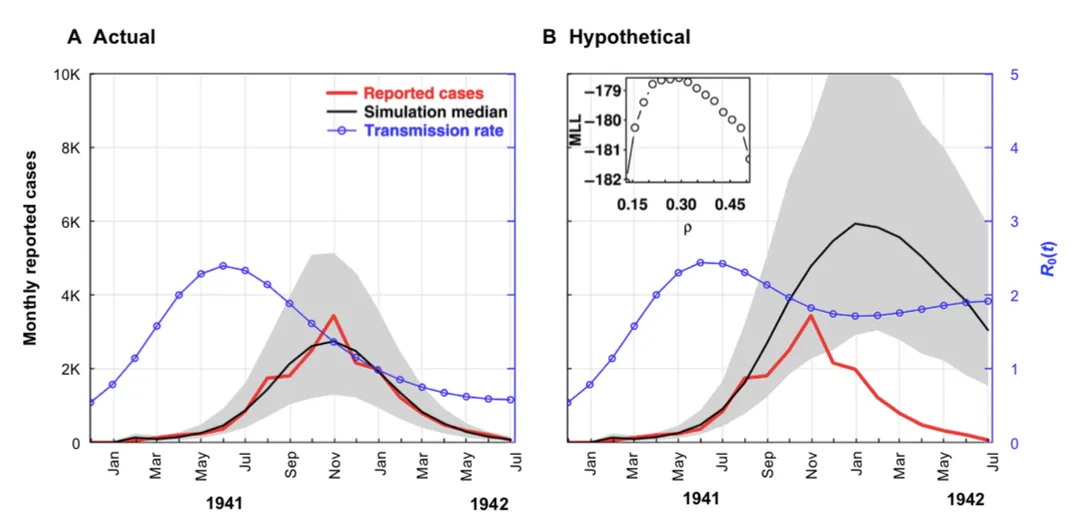
The researchers used a disease model where the estimated population of ghetto residents was divided into classes representing different individuals’ disease states: susceptible, exposed, infected or recovered. They then added a disease vector factor representing lice to the equation, using a rate of spread that would emulate any sort of external factor taking hold, like preventative public health measures. The model’s total median number of simulated reported and unreported cases over the period of September 1940 to July 1942 was approximately 72,000, with a possible maximum of 113,000 cases. When the researchers compared their run to the actual data available from a variety of reports and medical and historical accounts from the ghetto’s records, the numbers matched. Having shown the model was reliable, they next used it to predict the trajectory of the typhus spread with a constant rate of infection, which they would expect when no preventive measures are put in place. The run showed that cases would have exceeded 190,000, an outbreak two to three times higher than what occurred.
Since the number of susceptible Jews remained relatively high during the test run period, the authors said the epidemic was unlikely to have dropped for a lack of hosts. They concluded there must be other factors at play. “And so, we hypothesized that the epidemic crashed actually due to the community's efforts, which were substantial in the end to try to bring that epidemic down,” says Stone.
Among the Jewish public health officials working within the ghetto was epidemiologist Ludwik Hirszfeld, who co-discovered the inheritance of blood types. Hirszfeld had helped establish the National Institute of Hygiene in the Polish state that existed between the world wars and played a major role in establishing public health initiatives within the ghetto. In his memoir, Hirszfeld wrote, “typhus is the inseparable companion of war and famine… This disease destroys more people than ‘the most brilliant’ commander. It often decides the outcome of wars.”
To combat the deadly disease, even with scant resources, Hirszfeld and other Jewish doctors sponsored hundreds of public lectures, offered sanitary and hygiene courses, and set up an underground medical university to train young medical students on the co-occurring effects of starvation and epidemics. Because no antibiotic was available for typhus at the time, the best treatments included de-lousing and staying clean. Stone says doctors and public health workers encouraged people to monitor for lice, change and iron clothes and wash as much as possible. While those efforts extended throughout the ghetto, volunteer agencies took advantage of a meager influx of food that came after May 1941 and set up a feeding program that helped to moderately quell some of the starvation.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/48/96/48961a8d-4306-464c-9229-8e05ca54242f/jews_in_warsaw_ghetto_soup_kitchen.jpg)
Not everyone is convinced community health efforts fully explain the drop in disease. Samuel Kassow, historian and author of Who Will Write Our History? Rediscovering a Hidden Archive From the Warsaw Ghetto, says the current study is provocative, but that tactics encouraged by Jewish public health workers would have been challenging to enact. Due to the lack of coal as a fuel source, buildings had no heat and pipes froze, which made washing and staying clean very difficult. “How can you have ‘social distancing’ for example, when the Germans configured the ghetto in such a way that to get from A to B to C there were narrow ‘choke points’ where masses of people had to crowd against each other,” he says. “Imagine the staircases at Grand Central at 5 p.m. if all the escalators failed at once.”
While typhus had devastating effects in the ghetto, Frydel notes ways that righteous gentiles used public health information about typhus outside of the ghetto as a means to help save Jews in hiding. “We find moving stories of rescuers using typhus to scare off the German police,” he says.
Rescuers could keep authorities at bay by telling the Gestapo that typhus-infected individuals were inside. Some Polish doctors figured out how to forge positive tests to save lives. When workers with fake typhus-positive tests showed up to a factory or forced work site, Germans sent them home to quarantine, where they had a chance to escape being worked to exhaustion.
The case of the Warsaw ghetto is not the first or only example of the interplay between politics and disease, but the study does provide illuminating evidence in favor of the efficacy of public health campaigns and the need for novel ways to assess disease risk factors, especially in light of the ongoing coronavirus pandemic.
Lynn Goldman, the dean of George Washington University’s Milken Institute of Public Health, says the study’s combination of history, medicine, epidemiology and first-hand accounts is rare and the methodology could be hugely important to containing coronavirus and other diseases, especially in high-risk, low resource populations.
“Around the world, some refugee camps are as bad or worse, in terms of public health, and the ability to get in there and assess what's really going on and then to control pandemics is very difficult,” Goldman says. “This kind of paper, we could use it to teach humanitarian assistance, disaster response. But also, it could be used to teach history, to teach political science.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Sexton_Remy.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Sexton_Remy.jpg)