These “Sponges” Can Soak Up Cancer Cells
Implants designed to detect early metastasis can also trap cancer cells
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/f2/c2/f2c20afa-1e2a-40d9-aca0-a0baf815c6cb/20150805_bmecancerattractor_jx002_copy.jpg)
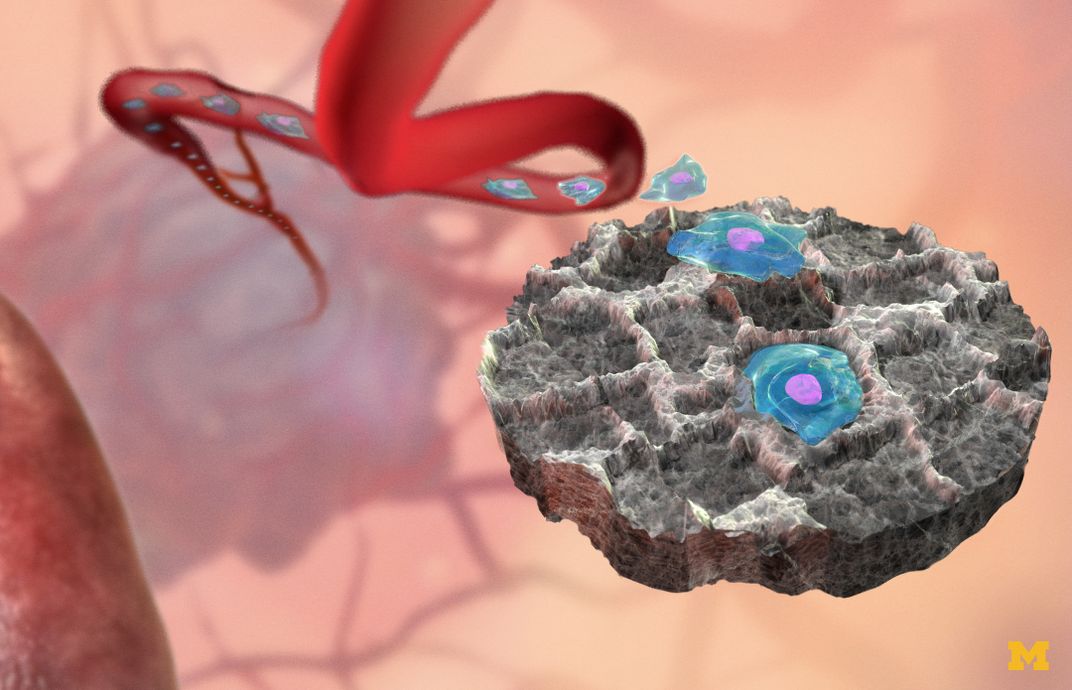
Early detection of metastatic cancer can mean the difference between life and death. To aid this, a group of researchers at the University of Michigan have developed tiny implantable mesh disks, which act like sponges. The so-called "scaffolds," made from the biomaterial polylactic-co-glycolide, collect the cancerous cells, so they can be detected and potentially eliminated.
“We know that we can get blood vessels and immune cells, which are critical for getting cancer cells, to collect," says Samira Azarin, the lead author on the study. "We found that when we implanted the scaffolds into the mice the tumor did all the work for us.”
Metastatic cancer, or cells that have traveled from the site of the original cancer to somewhere else in the body, has a hand in 90 percent of cancer deaths. The scientists were looking for a way to detect those cells right when they started metastasizing, so that they could be treated early.
The implants—5-milimeter by 2-milimeter tubes put under the skin near lymph nodes—collect metastatic cells by mimicking similar environments within the body where cells gather. The research group had previously been using them for tissue engineering, so they knew they were prime environments for cell growth. The tubes can be scanned using a non-invasive detection method called inverse spectroscopic optical coherence tomography (ISOCT), which shows early presence of tumor cells.
The team found the detection worked really well, and that they can scan the implants for nanoscale changes in cell buildup. But there were additional benefits, too. The scaffolds acted like sponges, soaking up the metastatic cells and preventing them from growing elsewhere in the body. According to the report, the scaffold “reduces the tumor burden within solid organs 10-fold.”
Azarin says she and her colleagues were hoping that might happen, as an added benefit to the study, but they were unsure until they actually started scanning the scaffolds. “The fact that in and of itself it could be therapeutic is an added bonus,” she says.
They tested the scaffolds on mice with breast cancer, because, like other similar cancers, it’s often not the initial tumor that kills the patient. It becomes deadly when it metastasizes to the brain, bones, liver or lungs.
“We wanted to look at the type of cancer where detection and treatment of the metastasis would be the most helpful,” Azarin says. “There’s many types of cancer where this is the case, and the problem with metastasis is that they go to really important organs. We’re also looking at ovarian and pancreatic cancer.”
The scientists are still testing the devices in mice, but Azarin says they're working with surgical oncologists to see how they might best be used in humans in the future.
At first, the sponges will likely be used by patients who have had a tumor removed and are in remission, to make sure their cancer doesn’t come back. Currently, a lot of patients don’t know their cancer has metastasized until they see symptoms, and by that time the cancer has often spread widely. Azarin says eventually the implants might be used for people who haven’t had previous cancers, but are in high-risk groups.
Now that the researchers know the implants can detect metastatic cancer in mice, they are looking to see if they can actually remove cancerous cells from the body. The sponges can also be used to study when cells metastasize and how different environments within the body impact that growth. “There’s not a lot you can do to modify an organ like a lung or liver, but with a scaffold we can really edit the site,” Azarin says.
The implant has huge potential, in large part because it’s simple and adaptable.
“It’s an FDA approved material, the scaffold is easy to make, and it’s inexpensive technology,” Azarin says. “What I learned in this process is that we tend to want to over-engineer things, but really sometimes simple materials and simple approaches work best.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/DSC_0196_2.JPG)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/DSC_0196_2.JPG)