The Insane and Exciting Future of the Bionic Body
From “i-limbs” to artificial organs, advances in technology have led to an explosion of innovation in the increasingly critical field of prosthetics
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/SEP13_E01_Prosthetics_631x300.jpg)
Bertolt Meyer pulls off his left forearm and gives it to me. It’s smooth and black, and the hand has a clear silicone cover, like an iPhone case. Beneath the rubbery skin are skeletal robotic fingers of the sort you might see in a sci-fi movie—the “cool factor,” Meyer calls it.
I hold the arm in my hand. “It’s pretty light,” I say. “Yes, only a couple of pounds,” he responds.
I try not to stare at the stump where his arm should be. Meyer explains how his prosthetic limb works. The device is held on by suction. A silicone sheath on the stump helps create a tight seal around the limb. “It needs to be comfortable and snug at the same time,” he says.
“Can I touch it?” I ask. “Go ahead,” he says. I run my hand along the sticky silicone and it helps dispel my unease—the stump may look strange, but the arm feels strong and healthy.
Meyer, 33, is slightly built and has dark features and a friendly face. A native of Hamburg, Germany, currently living in Switzerland, he was born with only an inch or so of arm below the left elbow. He has worn a prosthetic limb on and off since he was 3 months old. The first one was passive, just to get his young mind accustomed to having something foreign attached to his body. When he was 5 years old, he got a hook, which he controlled with a harness across his shoulders. He didn’t wear it much, until he joined the Boy Scouts when he was 12. “The downside is that it is extremely uncomfortable because you’re always wearing the harness,” he says.
This latest iteration is a bionic hand, with each finger driven by its own motor. Inside of the molded forearm are two electrodes that respond to muscular signals in the residual limb: Sending a signal to one electrode opens the hand and to the other closes it. Activating both allows Meyer to rotate the wrist an unnerving 360 degrees. “The metaphor that I use for this is learning how to parallel park your car,” he says as he opens his hand with a whir. At first, it’s a little tricky, but you get the hang of it.
Touch Bionics, the maker of this mechanical wonder, calls it the i-limb. The name represents more than marketing. Improved software, longer-lasting batteries and smaller, more power-efficient microprocessors—the technologies driving the revolution in personal electronics—have ushered in a new era in bionics. In addition to prosthetic limbs, which are more versatile and user-friendly than ever before, researchers have developed functioning prototypes of artificial organs that can take the place of one’s spleen, pancreas or lungs. And an experimental implant that wires the brain to a computer holds the promise of giving quadriplegics control over artificial limbs. Such bionic marvels will increasingly find their way into our lives and our bodies. We have never been so replaceable.
I met Meyer on a summer day in London, in the courtyard of a 19th- century cookie factory. Meyer is a social psychologist at the University of Zurich, but his personal experiences with prosthetics have instilled in him a fascination with bionic technology. He says the past five years, in particular, have seen an explosion of innovation. As we chatted over coffee, engineers worked on a novel demonstration in a nearby building. During the past few months, they had been gathering prosthetic limbs and artificial organs from around the world to be assembled into a single, artificial structure named the Bionic Man. You can see the startling results in a documentary airing October 20 on the Smithsonian Channel.
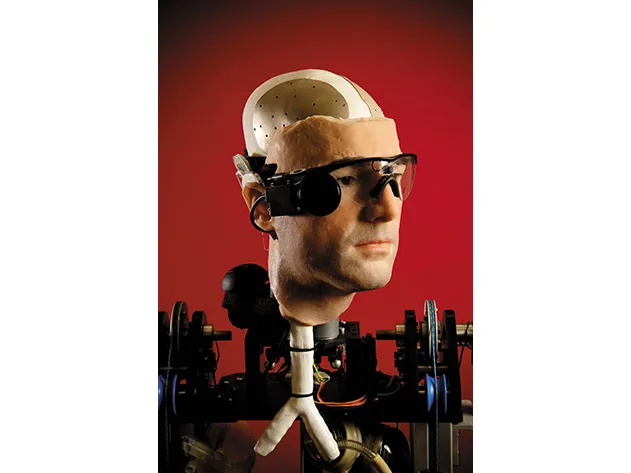
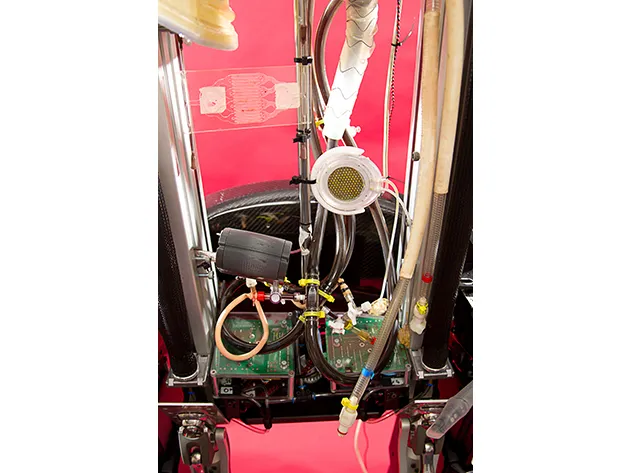
Engineers designed the Bionic Man to enable several of its human-dependent parts to operate without a body. For instance, although the robot is fitted with i-limbs, it doesn’t possess the nervous system or brain to make them work. Instead, the Bionic Man can be controlled remotely via a computer and specially designed interfacing hardware, while a Bluetooth connection can be used to operate the i-limbs. Nonetheless, the robot vividly showcases how much of our bodies can be replaced by circuits, plastic and metal. Adding to the dramatic effect, the Bionic Man’s face is a silicone replica of Meyer’s.
Rich Walker, the managing director of the project, says his team was able to rebuild more than 50 percent of the human body. The level of progress in bionics surprised not only him but “even the researchers who had worked on the artificial organs,” he says. Although multiple artificial organs can’t yet function together in a single human body, the scenario has become realistic enough that bioethicists, theologians and others are contending with the question, How much of a human being can be replaced and still be considered human? For many, the criterion is whether a device enhances or interferes with a patient’s ability to relate to other people. There’s broad agreement, for instance, that technology that restores motor functions to a stroke victim or provides sight to the blind does not make a person less human. But what about technology that could one day transform the brain into a semi-organic supercomputer? Or endow people with senses that perceive wavelengths of light, frequencies of sounds and even types of energy that are normally beyond our reach? Such people might no longer be described as strictly “human,” regardless of whether such enhancements represent an improvement over the original model.
These big questions seem far away when I first see engineers working on the Bionic Man. It is still a faceless collection of unassembled parts. Yet the arms and legs laid out on a long black table clearly evoke the human form.
Meyer himself speaks to that quality, describing his i-limb as the first prosthetic he has used in which the aesthetics match the engineering. It truly feels like part of him, he says.
David Gow, a Scottish engineer who created the i-limb, says one of the most significant accomplishments in the field of prosthetics has been making amputees feel whole again, and no longer embarrassed to be seen wearing an artificial limb. “Patients actually want to shake people’s hands with it,” he says.
Gow, 56, has long been fascinated by the challenge of designing prosthetics. After briefly working in the defense industry he became an engineer at a government research hospital attempting to develop electrically powered prosthetics. He had one of his first breakthroughs while trying to figure out how to design a hand small enough for children. Instead of employing one central motor, the standard approach, he incorporated smaller motors into the thumb and fingers. The innovation both reduced the size of the hand and paved the way for articulated digits.
That modular design later became the basis for the i-limb: Each finger is powered by a 0.4-inch motor that automatically shuts down when sensors indicate sufficient pressure is applied to whatever is being held. Not only does that prevent the hand from crushing, say, a foam cup, it allows for a variety of grips. When the fingers and thumb are lowered together, they create a “power grip” for carrying large objects. Another grip is formed by closing the thumb on the side of the index finger, allowing the user to hold a plate or (rotating the wrist) turn a key in a lock. A technician or user can program the i-limb’s small computer with a menu of preset grip configurations, each of which is triggered by a specific muscle movement that requires extensive training and practice to learn. The latest iteration of the i-limb, released this past April, goes a step farther: An app loaded onto an iPhone gives users access to a menu of 24 different preset grips with the touch of a button.
To Hugh Herr, a biophysicist and engineer who is the director of the biomechatronics group at the Massachusetts Institute of Technology’s Media Lab, prosthetics are improving so quickly that he predicts disabilities will be largely eliminated by the end of the 21st century. If so, it will be in no small part thanks to Herr himself. He was 17 years old when he was caught in a blizzard while climbing New Hampshire’s Mount Washington in 1982. He was rescued after three-and-a-half days, but by then frostbite had taken its toll, and surgeons had to amputate both his legs below the knees. He was determined to go mountain climbing again, but the rudimentary prosthetic legs he had been fitted with were only capable of slow walking. So Herr designed his own legs, optimizing them to maintain balance on mountain ledges as narrow as a dime. More than 30 years later, he holds or co-holds more than a dozen patents related to prosthetic technologies, including a computer-controlled artificial knee that automatically adapts to different walking speeds.
Herr personally uses eight different kinds of specialized prosthetic legs, designed for activities that include running, ice climbing and swimming. It’s extremely difficult, he says, to design a single prosthetic limb “to do many tasks as well as the human body.” But he believes that a prosthesis capable of “both walking and running that performs at the level of the human leg” is just one or two decades away.
***
The oldest known prosthetics were used some 3,000 years ago in Egypt, where archaeologists have unearthed a carved wooden toe attached to a piece of leather that could be fitted onto a foot. Functional mechanical limbs didn’t come along until the 16th century, when a French battlefield surgeon named Ambroise Paré invented a hand with flexible fingers operated by catches and springs. He also built a leg with a mechanical knee that the user could lock into place while standing. But such advances were the exception. Throughout most of human history, a person who lost a limb was likely to succumb to infection and die. A person born without a limb was typically shunned.
In the United States, it was the Civil War that first put prosthetics into widespread use. Amputating a shattered arm or leg was the best way to prevent gangrene, and it took a practiced surgeon just minutes to administer chloroform, lop off the limb and sew the flap shut. Around 60,000 amputations were performed by both North and South, with a 75 percent survival rate. After the war, when the demand for prosthetics skyrocketed, the government stepped in, providing veterans with money to pay for new limbs. Subsequent wars led to more advances. In World War I, 67,000 amputations took place in Germany alone, and doctors there developed new arms that could enable veterans to return to manual labor and factory work. Following World War II, new materials such as plastics and titanium made their way into artificial limbs. “You can find major innovations after every period of war and conflict,” says Herr.
The wars in Iraq and Afghanistan are no exception. Since 2006, the Defense Advanced Research Projects Agency has put some $144 million into prosthetic research to help the estimated 1,800 U.S. soldiers who have suffered traumatic limb loss.
Some of that investment went to Herr’s most prominent invention, a bionic ankle designed for people who have lost one or both legs below the knees. Known as the BiOM and sold by Herr’s company iWalk (there are a lot of lowercase “i’s” floating around the prosthetics industry these days), the device—fitted with sensors, multiple microprocessors and a battery—propels users forward with each step, helping amputees regain lost energy as they walk. Roy Aaron, a professor of orthopedic surgery at Brown University and the director of the Brown/VA Center for Restorative and Regenerative Medicine, says people who use a BiOM compare it to striding on a moving walkway at an airport.
Herr envisions a future where prosthetics such as the BiOM can be merged with the human body. Amputees who sometimes have to endure chafing and sores while wearing their devices might one day be able to attach their artificial limbs directly to their bones with a titanium rod.
Michael McLoughlin, the engineer leading development of advanced prosthetics at the Johns Hopkins University Applied Physics Laboratory, also wants to see bionic limbs that are more integrated with the human body. The Modular Prosthetic Limb (MPL), an artificial arm-and-hand mechanism that was built by the Johns Hopkins lab, has 26 joints controlled by 17 separate motors and “can do just about everything a normal limb can do,” says McLoughlin. But the MPL’s sophisticated movements are limited by the level of technology available for interfacing with the body’s nervous system. (It’s comparable to owning a top-of-the-line personal computer that’s hooked up to a slow Internet connection.) What’s needed is a way to increase the data flow—possibly by establishing a direct uplink to the brain itself.
In April 2011, researchers at Brown achieved just that when they connected a robotic arm directly into the mind of Cathy Hutchinson, a 58-year-old quadriplegic who is unable to move her arms and legs. The results, captured on video, are astounding: Cathy can pick up a bottle and lift it to her mouth to drink.
This feat was made possible when neurosurgeons created a small hole in Cathy’s skull and implanted a sensor the size of a baby aspirin into her motor cortex, which controls body movements. On the outside of the sensor are 96 hair-thin electrodes that can detect electrical signals emitted by neurons. When a person thinks about performing a specific physical task—such as lifting her left arm or grabbing a bottle with her right hand—the neurons emit a distinct pattern of electrical pulses associated with that motion. In Hutchinson’s case, neuroscientists first asked her to imagine a series of body movements; with each mental effort, the electrodes implanted in her brain picked up the electrical pattern generated by the neurons and transmitted it through a cable to an external computer near her wheelchair. Next, the researchers translated each pattern into a command code for a robotic arm mounted on the computer, allowing her to control the mechanical hand with her mind. “The whole study is embodied in one frame of the video, and that is Cathy’s smile when she puts the bottle down,” says Brown neuroscientist John Donoghue, who co-directs the research program.
Donoghue hopes this study will eventually make it possible for the brain to form a direct interface with bionic limbs. Another goal is to develop an implant that can record and transmit data wirelessly. Doing so would eliminate the cord that presently connects the brain to the computer, allowing mobility for the user and lowering the risk of infection that results from wires passing through the skin.
Perhaps the toughest challenge faced by inventors of artificial organs is the body’s defense system. “If you put something in, the whole body’s immune system will try to isolate it,” says Joan Taylor, a professor of pharmaceutics at De Montfort University in England, who is developing an artificial pancreas. Her ingenious device contains no circuitry, batteries or moving parts. Instead, a reservoir of insulin is regulated by a unique gel barrier that Taylor invented. When glucose levels rise, the excess glucose in the body’s tissues infuse the gel, causing it to soften and release insulin. Then, as glucose levels drop, the gel re-hardens, reducing the release of insulin. The artificial pancreas, which would be implanted between the lowest rib and the hip, is connected by two thin catheters to a port that lies just beneath the skin’s surface. Every few weeks, the reservoir of insulin would be refilled using a
syringe that fits into the port.
The challenge is, when Taylor tested the device in pigs, the animals’ immune system responded by forming scar tissue known as adhesions. “They are like glue on internal organs,” Taylor says, “causing constrictions that can be painful and lead to serious problems.” Still, diabetes is such a widespread problem—as many as 26 million Americans are afflicted—that Taylor is testing the artificial pancreas in animals with an eye toward solving the rejection problem before beginning clinical trials with people.
For some manufacturers of artificial organs, the main problem is blood. When it encounters something foreign, it clots. It’s a particular obstacle to crafting an effective artificial lung, which must pass blood through tiny synthetic tubes. Taylor and other researchers are teaming up with biomaterial specialists and surgeons who are developing new coatings and techniques to improve the body’s acceptance of foreign material. “I think with more experience and expert help, it can be done,” she says. But before Taylor can continue her research, she says she needs to find a partner to provide more funding.
And private investors can be hard to come by, since it may take years to achieve the technological breakthroughs that make an invention profitable. SynCardia Systems, an Arizona company that makes an artificial heart device capable of pumping up to 2.5 gallons of blood per minute, was founded in 2001 but wasn’t in the black until 2011. It recently developed a portable battery-powered compressor weighing only 13.5 pounds that allows a patient to leave the confines of a hospital. The FDA has approved the SynCardia Total Artificial Heart for patients with end-stage biventricular failure who are waiting for a heart transplant.
Makers of bionic arms and legs also fight an uphill financial battle. “You have a high-end product with a small market and that does make it challenging,” says McLoughlin. “This is not like investing in a Facebook or a Google; you’re not going to make your billions by investing in prosthetic limbs.” Meanwhile, government money for advanced prosthetics could get tighter in coming years. “As the wars wind down, funding for this kind of research is going to drop off,” orthopedic surgeon Roy Aaron predicts.
Then there’s the cost of purchasing a prosthetic limb or artificial organ. A recent study published by the Worcester Polytechnic Institute found that robotic upper limb prosthetics cost $20,000 to $120,000. Although some private insurance companies will cover 50 to 80 percent of the fee, others have payment caps or cover only one device in a patient’s lifetime. Insurance companies are also known to question whether the most advanced prosthetics are “medically necessary.”
Herr believes that insurance providers need to radically rethink their cost-benefit analyses. Although the latest bionic prosthetics are more expensive per unit than less-complex devices, he argues, they reduce health care payouts across the lifetime of the patient. “When leg amputees use low-tech prostheses, they develop joint conditions, knee arthritis, hip arthritis, and they’re on continual pain medication,” says Herr. “They don’t walk that much because walking is difficult, and that drives cardiovascular disease and obesity.”
Other trends, however, suggest that artificial limbs and organs may continue to improve and become more affordable. In the developed world, people are living longer than ever, and they are increasingly facing failures of one body part or another. The number one cause of lower-limb amputation in the United States is not war but diabetes, which in its later stages—especially among the elderly—can hamper circulation to the extremities. Moreover, Donoghue believes the brain-prosthetic interface he’s working on could be used by stroke patients and people with neurodegenerative diseases to help restore some degree of normalcy to their lives. “We’re not there yet,” Donoghue admits, adding: “There will come a time when a person has a stroke and if we can’t repair it biologically, there will be an option to get a technology that will rewire their brain.”
Most of those technologies are still years away, but if anyone will benefit it will be Patrick Kane, a talkative 15-year-old with chunky glasses and wispy blond hair. Shortly after birth, he was stricken by a massive infection that forced doctors to remove his left arm and part of his right leg below the knee. Kane is one of the youngest persons to be fitted with an i-limb prosthetic of the sort Meyer showed me.
The thing Kane likes most is the way it makes him feel. “Before, the looks I got were an ‘Oh, what happened to him? Poor him,’ sort of thing,” he says as we sit in a London café. “Now, it’s ‘Ooh? What’s that? That’s cool!’” As if on cue, an elderly man at the next table chimes in: “I gotta tell you something, it looks amazing. It’s like a Batman arm!” Kane does a demonstration for the man. Such technology is as much about changing the way people see him as it is about changing what he can do.
I ask Kane about some of the far-out advances that might be available to him in the coming decades. Would he want a limb that was bolted to his skeletal system? Not really. “I like the idea that I can take it off and be me again,” he says. What about a prosthetic arm that could directly interface with his brain? “I think that would be very interesting,” he says. But he would worry about something going wrong.
Depending on what happens next, Kane’s future may be filled with technological marvels—new hands and feet that bring him closer to, or even beyond, the capabilities of a so-called able-bodied person. Or progress might not come so fast. As I watch him dart across the road to the bus stop, it occurs to me that he’ll be fine either way.