Keeping Vaccines Safe in Tiny “Cages”
By encasing vaccines in silica, researchers could eliminate the need to refrigerate them during transportation
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/9d/b5/9db5de28-1c79-4bfa-bdd5-7acd2cb8327d/proteins.jpg)
Asel Sartbaeva was taking her young daughter to the doctor for her childhood vaccines—a ritual familiar to most new parents—when something caught her attention. The doctor took the vaccine out of the refrigerator and administered it immediately, while it was still cold.
“I asked, sort of naively, why shouldn’t we wait for it to warm up,” Sartbaeva recalls. “The doctor said ‘no, no, no if you let it warm up it will spoil.”
Most parents would leave it at that. But Sartbaeva is a materials scientist, and the properties of different things in the world are inherently interesting to her. She went home and Googled what vaccines are made of, and why they need to be kept cold. The answer, she discovered, is that most vaccines contain proteins that break down at room temperature. And she learned something more shocking too—keeping vaccines cold during transport through the developed world is so challenging that some 40 percent of all vaccine doses are ruined before they can be used.
“I was just appalled with the numbers of how many vaccines are wasted today,” she says.
So Sartbaeva, who is part of the chemistry department at the University of Bath, decided to do something about it. She’s spent the past three years developing a method of using silica—the base material for sand and glass—to create tiny “cages” around the vaccine proteins. The silica binds around the proteins, conforming to their shapes to create multiple layers of protection. The process, which was just published in the journal Scientific Reports, can keep the proteins intact at temperatures of up to 100 degrees Celsius. The proteins will also stay intact for up to three years at room temperature. Then, when the vaccines reach their destination, the silica cages can be washed off using a chemical process.
Sartbaeva and her team, who have named the process “ensilication,” hope it will save millions of dollars in refrigerated transport and in wasted vaccines. This could allow vaccines to reach places with a lack of infrastructure that makes refrigeration difficult.
“If we could reduce the cost, it would be a tremendous achievement,” she says. “And if we can safely deliver vaccines without refrigeration, than people who don’t have access to vaccines today will be able to get them.”
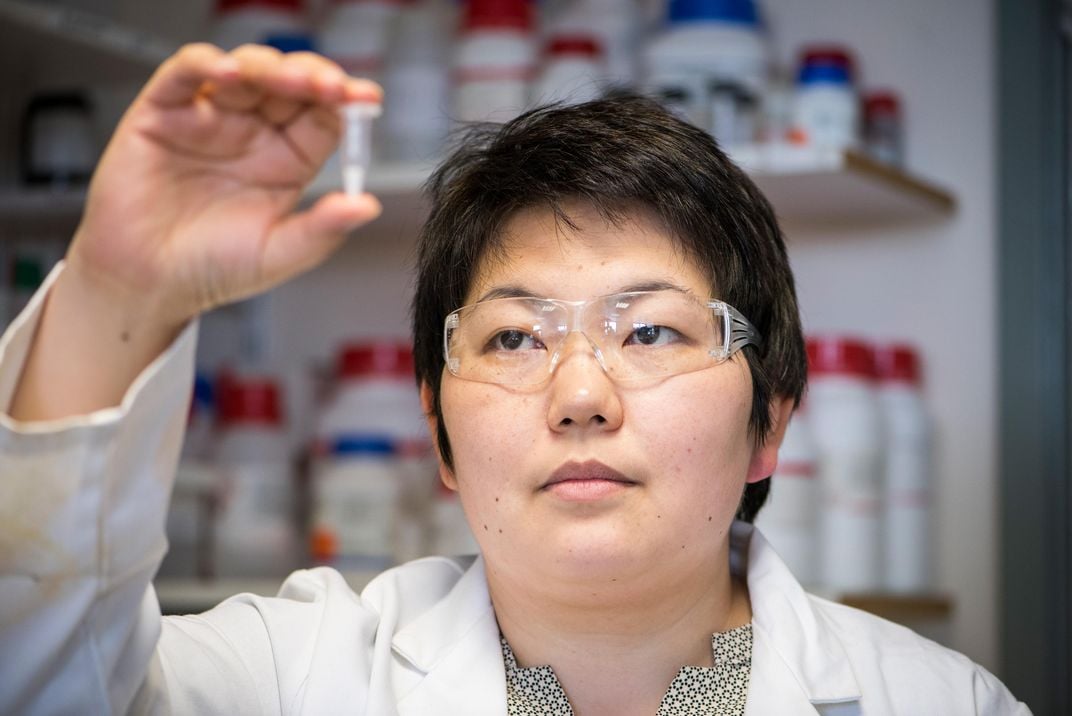
Sartbaeva and her team have tested the process on the tetanus toxoid, the protein used in the tetanus vaccine. They also tested it on two other proteins—horse hemoglobin and an enzyme from egg whites. The process works on protein-based vaccines, including all the common childhood vaccines, such as the DTaP (diphtheria, tetanus and pertussis), the MMR (measles, mumps and rubella) and the pneumococcal vaccine, which can prevent pneumonia, sepsis and meningitis. It does not work on the newer category of DNA vaccines, which are currently under investigation but not yet on the market.
The team has begun animal trials, the results of which will be published in a second paper.
The next step for Sartbaeva is to perfect a mechanical method for removing the silica from the vaccine proteins, making chemical washing unnecessary. They’re currently working on a method involving shaking the vaccine vigorously enough to break the silica’s covalent bonds. The material can then be filtered to separate the silica from the protein. They’ve been getting good results, Sartbaeva says, but they need to shorten the process from 20 minutes to 1 or 2 before it’s practical to use in a medical setting. They’re also actively looking for pharmaceutical companies to partner with.
For Sartbaeva, who has been working with silica for 15 years, seeing the process work has been enormously exciting but also nerve-wracking. Silica had never been used in this capacity, and each failure in the experimenting process filled Sartbaeva with self-doubt.
“When it didn’t work, I said ‘OK, maybe this is crazy, maybe I should stop,’” she says. “I think the hardest thing was really believing it would work.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/matchar.png)

/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/matchar.png)