How the Horrific 1918 Flu Spread Across America
The toll of history’s worst epidemic surpasses all the military deaths in World War I and World War II combined. And it may have begun in the United States
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/df/e6/dfe66606-c372-429a-9ab2-80e7754f5d6d/nov2017_e02_fluhistory1918.jpg)
Haskell County, Kansas, lies in the southwest corner of the state, near Oklahoma and Colorado. In 1918 sod houses were still common, barely distinguishable from the treeless, dry prairie they were dug out of. It had been cattle country—a now bankrupt ranch once handled 30,000 head—but Haskell farmers also raised hogs, which is one possible clue to the origin of the crisis that would terrorize the world that year. Another clue is that the county sits on a major migratory flyway for 17 bird species, including sand hill cranes and mallards. Scientists today understand that bird influenza viruses, like human influenza viruses, can also infect hogs, and when a bird virus and a human virus infect the same pig cell, their different genes can be shuffled and exchanged like playing cards, resulting in a new, perhaps especially lethal, virus.
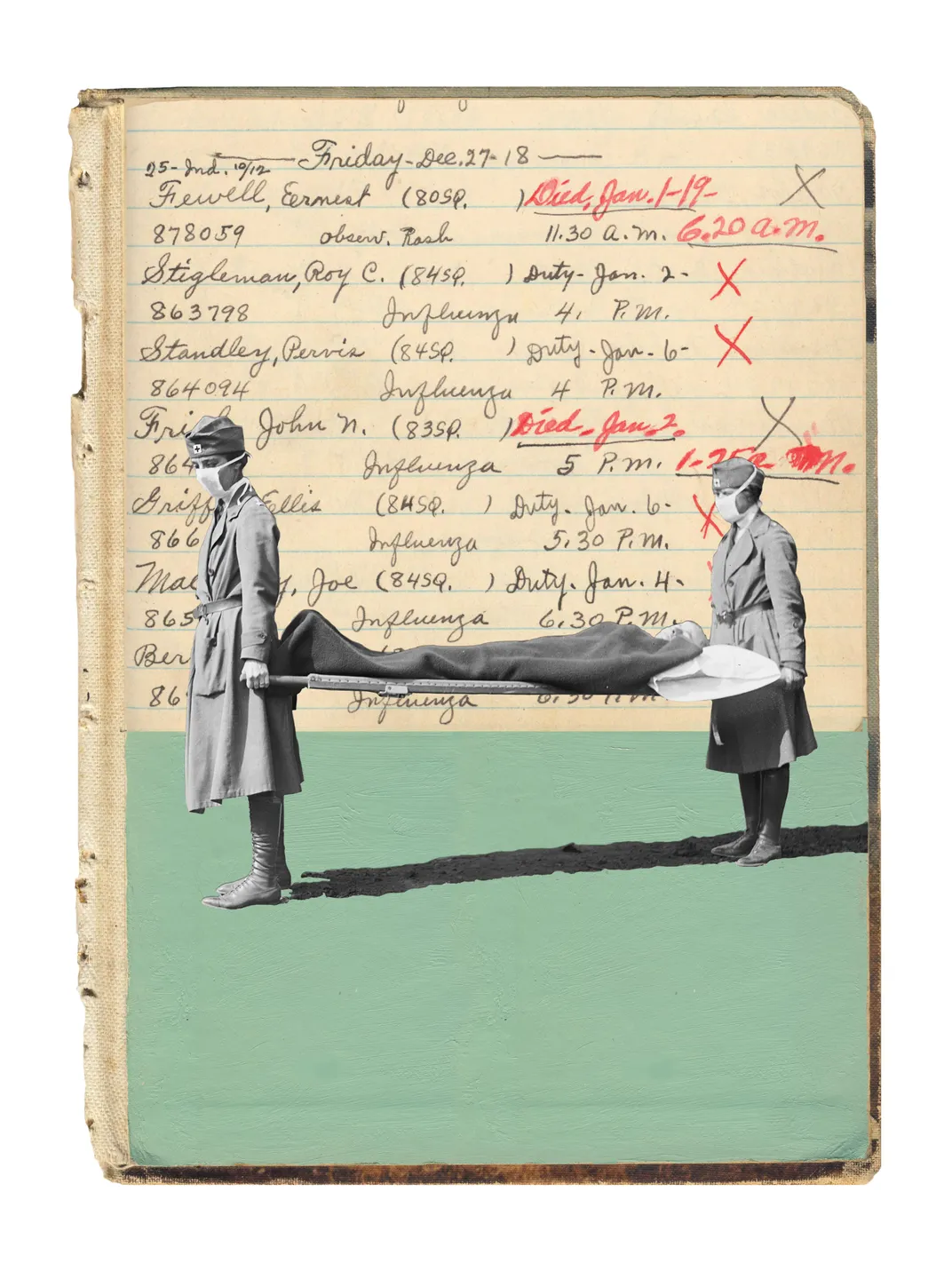
We cannot say for certain that that happened in 1918 in Haskell County, but we do know that an influenza outbreak struck in January, an outbreak so severe that, although influenza was not then a “reportable” disease, a local physician named Loring Miner—a large and imposing man, gruff, a player in local politics, who became a doctor before the acceptance of the germ theory of disease but whose intellectual curiosity had kept him abreast of scientific developments—went to the trouble of alerting the U.S. Public Health Service. The report itself no longer exists, but it stands as the first recorded notice anywhere in the world of unusual influenza activity that year. The local newspaper, the Santa Fe Monitor, confirms that something odd was happening around that time: “Mrs. Eva Van Alstine is sick with pneumonia...Ralph Lindeman is still quite sick...Homer Moody has been reported quite sick...Pete Hesser’s three children have pneumonia ...Mrs J.S. Cox is very weak yet...Ralph Mc-Connell has been quite sick this week...Mertin, the young son of Ernest Elliot, is sick with pneumonia,...Most everybody over the country is having lagrippe or pneumonia.”
Several Haskell men who had been exposed to influenza went to Camp Funston, in central Kansas. Days later, on March 4, the first soldier known to have influenza reported ill. The huge Army base was training men for combat in World War I, and within two weeks 1,100 soldiers were admitted to the hospital, with thousands more sick in barracks. Thirty-eight died. Then, infected soldiers likely carried influenza from Funston to other Army camps in the States—24 of 36 large camps had outbreaks—sickening tens of thousands, before carrying the disease overseas. Meanwhile, the disease spread into U.S. civilian communities.
The influenza virus mutates rapidly, changing enough that the human immune system has difficulty recognizing and attacking it even from one season to the next. A pandemic occurs when an entirely new and virulent influenza virus, which the immune system has not previously seen, enters the population and spreads worldwide. Ordinary seasonal influenza viruses normally bind only to cells in the upper respiratory tract—the nose and throat—which is why they transmit easily. The 1918 pandemic virus infected cells in the upper respiratory tract, transmitting easily, but also deep in the lungs, damaging tissue and often leading to viral as well as bacterial pneumonias.
Although some researchers argue that the 1918 pandemic began elsewhere, in France in 1916 or China and Vietnam in 1917, many other studies indicate a U.S. origin. The Australian immunologist and Nobel laureate Macfarlane Burnet, who spent most of his career studying influenza, concluded the evidence was “strongly suggestive” that the disease started in the United States and spread to France with “the arrival of American troops.” Camp Funston had long been considered as the site where the pandemic started until my historical research, published in 2004, pointed to an earlier outbreak in Haskell County.
Wherever it began, the pandemic lasted just 15 months but was the deadliest disease outbreak in human history, killing between 50 million and 100 million people worldwide, according to the most widely cited analysis. An exact global number is unlikely ever to be determined, given the lack of suitable records in much of the world at that time. But it’s clear the pandemic killed more people in a year than AIDS has killed in 40 years, more than the bubonic plague killed in a century.
The impact of the pandemic on the United States is sobering to contemplate: Some 670,000 Americans died.
In 1918, medicine had barely become modern; some scientists still believed “miasma” accounted for influenza’s spread. With medicine’s advances since then, laypeople have become rather complacent about influenza. Today we worry about Ebola or Zika or MERS or other exotic pathogens, not a disease often confused with the common cold. This is a mistake.
We are arguably as vulnerable—or more vulnerable—to another pandemic as we were in 1918. Today top public health experts routinely rank influenza as potentially the most dangerous “emerging” health threat we face. Earlier this year, upon leaving his post as head of the Centers for Disease Control and Prevention, Tom Frieden was asked what scared him the most, what kept him up at night. “The biggest concern is always for an influenza pandemic...[It] really is the worst-case scenario.” So the tragic events of 100 years ago have a surprising urgency—especially since the most crucial lessons to be learned from the disaster have yet to be absorbed.
**********
Initially the 1918 pandemic set off few alarms, chiefly because in most places it rarely killed, despite the enormous numbers of people infected. Doctors in the British Grand Fleet, for example, admitted 10,313 sailors to sick bay in May and June, but only 4 died. It had hit both warring armies in France in April, but troops dismissed it as “three-day fever.” The only attention it got came when it swept through Spain, and sickened the king; the press in Spain, which was not at war, wrote at length about the disease, unlike the censored press in warring countries, including the United States. Hence it became known as “Spanish flu.” By June influenza reached from Algeria to New Zealand. Still, a 1927 study concluded, “In many parts of the world the first wave either was so faint as to be hardly perceptible or was altogether lacking...and was everywhere of a mild form.” Some experts argued that it was too mild to be influenza.
Yet there were warnings, ominous ones. Though few died in the spring, those who did were often healthy young adults—people whom influenza rarely kills. Here and there, local outbreaks were not so mild. At one French Army post of 1,018 soldiers, 688 were hospitalized and 49 died—5 percent of that population of young men, dead. And some deaths in the first wave were overlooked because they were misdiagnosed, often as meningitis. A puzzled Chicago pathologist observed lung tissue heavy with fluid and “full of hemorrhages” and asked another expert if it represented “a new disease.”

By July it didn’t seem to matter. As a U.S. Army medical bulletin reported from France, the “epidemic is about at an end...and has been throughout of a benign type.” A British medical journal stated flatly that influenza “has completely disappeared.”
In fact, it was more like a great tsunami that initially pulls water away from the shore—only to return in a towering, overwhelming surge. In August, the affliction resurfaced in Switzerland in a form so virulent that a U.S. Navy intelligence officer, in a report stamped “Secret and Confidential,” warned “that the disease now epidemic throughout Switzerland is what is commonly known as the black plague, although it is designated as Spanish sickness and grip.”
The second wave had begun.
**********
The hospital at Camp Devens, an Army training base 35 miles from Boston that teemed with 45,000 soldiers, could accommodate 1,200 patients. On September 1, it held 84.
On September 7, a soldier sent to the hospital delirious and screaming when touched was diagnosed with meningitis. The next day a dozen more men from his company were diagnosed with meningitis. But as more men fell ill, physicians changed the diagnosis to influenza. Suddenly, an Army report noted, “the influenza...occurred as an explosion.”
At the outbreak’s peak, 1,543 soldiers reported ill with influenza in a single day. Now, with hospital facilities overwhelmed, with doctors and nurses sick, with too few cafeteria workers to feed patients and staff, the hospital ceased accepting patients, no matter how ill, leaving thousands more sick and dying in barracks.
Roy Grist, a physician at the hospital, wrote a colleague, “These men start with what appears to be an ordinary attack of LaGrippe or Influenza, and when brought to the Hosp. they very rapidly develop the most vicious type of Pneumonia that has ever been seen. Two hours after admission they have the Mahogany spots over the cheek bones, and a few hours later you can begin to see the Cyanosis”—the term refers to a person turning blue from lack of oxygen—“extending from their ears and spreading all over the face....It is only a matter of a few hours then until death comes...It is horrible....We have been averaging about 100 deaths per day...For several days there were no coffins and the bodies piled up something fierce...”
Devens, and the Boston area, was the first place in the Americas hit by the pandemic’s second wave. Before it ended, influenza was everywhere, from ice-bound Alaska to steaming Africa. And this time it was lethal.
**********
The killing created its own horrors. Governments aggravated them, partly because of the war. For instance, the U.S. military took roughly half of all physicians under 45—and most of the best ones.
What proved even more deadly was the government policy toward the truth. When the United States entered the war, Woodrow Wilson demanded that “the spirit of ruthless brutality...enter into the very fibre of national life.” So he created the Committee on Public Information, which was inspired by an adviser who wrote, “Truth and falsehood are arbitrary terms....The force of an idea lies in its inspirational value. It matters very little if it is true or false.”
At Wilson’s urging, Congress passed the Sedition Act, making it punishable with 20 years in prison to “utter, print, write or publish any disloyal, profane, scurrilous, or abusive language about the form of government of the United State...or to urge, incite, or advocate any curtailment of production in this country of any thing or things...necessary or essential to the prosecution of the war.” Government posters and advertisements urged people to report to the Justice Department anyone “who spreads pessimistic stories...cries for peace, or belittles our effort to win the war.”
Against this background, while influenza bled into American life, public health officials, determined to keep morale up, began to lie.
Early in September, a Navy ship from Boston carried influenza to Philadelphia, where the disease erupted in the Navy Yard. The city’s public health director, Wilmer Krusen, declared that he would “confine this disease to its present limits, and in this we are sure to be successful. No fatalities have been recorded. No concern whatever is felt.”
The next day two sailors died of influenza. Krusen stated they died of “old-fashioned influenza or grip,” not Spanish flu. Another health official declared, “From now on the disease will decrease.”
The next day 14 sailors died—and the first civilian. Each day the disease accelerated. Each day newspapers assured readers that influenza posed no danger. Krusen assured the city he would “nip the epidemic in the bud.”
By September 26, influenza had spread across the country, and so many military training camps were beginning to look like Devens that the Army canceled its nationwide draft call.
Philadelphia had scheduled a big Liberty Loan parade for September 28. Doctors urged Krusen to cancel it, fearful that hundreds of thousands jamming the route, crushing against each other for a better view, would spread disease. They convinced reporters to write stories about the danger. But editors refused to run them, and refused to print letters from doctors. The largest parade in Philadelphia’s history proceeded on schedule.
The incubation period of influenza is two to three days. Two days after the parade, Krusen conceded that the epidemic “now present in the civilian population was...assuming the type found in” Army camps. Still, he cautioned not to be “panic stricken over exaggerated reports.”
He needn’t have worried about exaggeration; the newspapers were on his side. “Scientific Nursing Halting Epidemic,” an Inquirer headline blared. In truth, nurses had no impact because none were available: Out of 3,100 urgent requests for nurses submitted to one dispatcher, only 193 were provided. Krusen finally and belatedly ordered all schools closed and banned all public gatherings—yet a newspaper nonsensically said the order was not “a public health measure” and “there is no cause for panic or alarm.”
There was plenty of cause. At its worst, the epidemic in Philadelphia would kill 759 people...in one day. Priests drove horse-drawn carts down city streets, calling upon residents to bring out their dead; many were buried in mass graves. More than 12,000 Philadelphians died—nearly all of them in six weeks.
Across the country, public officials were lying. U.S. Surgeon General Rupert Blue said, “There is no cause for alarm if precautions are observed.” New York City’s public health director declared “other bronchial diseases and not the so-called Spanish influenza...[caused] the illness of the majority of persons who were reported ill with influenza.” The Los Angeles public health chief said, “If ordinary precautions are observed there is no cause for alarm.”
For an example of the press’s failure, consider Arkansas. Over a four-day period in October, the hospital at Camp Pike admitted 8,000 soldiers. Francis Blake, a member of the Army’s special pneumonia unit, described the scene: “Every corridor and there are miles of them with double rows of cots ...with influenza patients...There is only death and destruction.” Yet seven miles away in Little Rock, a headline in the Gazette pretended yawns: “Spanish influenza is plain la grippe—same old fever and chills.”
People knew this was not the same old thing, though. They knew because the numbers were staggering—in San Antonio, 53 percent of the population got sick with influenza. They knew because victims could die within hours of the first symptoms—horrific symptoms, not just aches and cyanosis but also a foamy blood coughed up from the lungs, and bleeding from the nose, ears and even eyes. And people knew because towns and cities ran out of coffins.
People could believe nothing they were being told, so they feared everything, particularly the unknown. How long would it last? How many would it kill? Who would it kill? With the truth buried, morale collapsed. Society itself began to disintegrate.
In most disasters, people come together, help each other, as we saw recently with Hurricanes Harvey and Irma. But in 1918, without leadership, without the truth, trust evaporated. And people looked after only themselves.
In Philadelphia, the head of Emergency Aid pleaded, “All who are free from the care of the sick at home... report as early as possible...on emergency work.” But volunteers did not come. The Bureau of Child Hygiene begged people to take in—just temporarily—children whose parents were dying or dead; few replied. Emergency Aid again pleaded, “We simply must have more volunteer helpers....These people are almost all at the point of death. Won’t you...come to our help?” Still nothing. Finally, Emergency Aid’s director turned bitter and contemptuous: “Hundreds of women...had delightful dreams of themselves in the roles of angels of mercy...Nothing seems to rouse them now...There are families in which the children are actually starving because there is no one to give them food. The death rate is so high and they still hold back.”
Philadelphia’s misery was not unique. In Luce County, Michigan, a couple and three children were all sick together, but, a Red Cross worker reported, “Not one of the neighbors would come in and help. I ...telephoned the woman’s sister. She came and tapped on the window, but refused to talk to me until she had gotten a safe distance away.” In New Haven, Connecticut, John Delano recalled, “Normally when someone was sick in those days [people] would bring food over to other families but...Nobody was coming in, nobody would bring food in, nobody came to visit.” In Perry County, Kentucky, the Red Cross chapter chairman begged for help, pleaded that there were “hundreds of cases...[of] people starving to death not from lack of food but because the well were panic stricken and would not go near the sick.”
In Goldsboro, North Carolina, Dan Tonkel recalled, “We were actually almost afraid to breathe...You were afraid even to go out...The fear was so great people were actually afraid to leave their homes...afraid to talk to one another.” In Washington, D.C., William Sardo said, “It kept people apart...You had no school life, you had no church life, you had nothing...It completely destroyed all family and community life...The terrifying aspect was when each day dawned you didn’t know whether you would be there when the sun set that day.”
An internal American Red Cross report concluded, “A fear and panic of the influenza, akin to the terror of the Middle Ages regarding the Black Plague, [has] been prevalent in many parts of the country.”
Fear emptied places of employment, emptied cities. Shipbuilding workers throughout the Northeast were told they were as important to the war effort as soldiers at the front. Yet at the L.H. Shattuck Co. only 54 percent of its workers showed up; at the George A. Gilchrist yard only 45 percent did; at Freeport Shipbuilding only 43 percent; at Groton Iron Works, 41 percent.
Fear emptied the streets, too. A medical student working in an emergency hospital in Philadelphia, one of the nation’s largest cities, encountered so few cars on the road he took to counting them. One night, driving the 12 miles home, he saw not a single car. “The life of the city had almost stopped,” he said.
On the other side of the globe, in Wellington, New Zealand, another man stepped outside his emergency hospital and found the same thing: “I stood in the middle of Wellington City at 2 P.M. on a weekday afternoon, and there was not a soul to be seen; no trams running; no shops open, and the only traffic was a van with a white sheet tied to the side with a big red cross painted on it, serving as an ambulance or hearse. It was really a city of the dead.”
Victor Vaughan, formerly the dean of the University of Michigan’s Medical School, was not a man to resort to hyperbole. Now the head of the Army’s communicable disease division, he jotted down his private fear: “If the epidemic continues its mathematical rate of acceleration, civilization could easily disappear...from the face of the earth within a matter of a few more weeks.”
**********
Then, as suddenly as it came, influenza seemed to disappear. It had burned through the available fuel in a given community. An undercurrent of unease remained, but aided by the euphoria accompanying the end of the war, traffic returned to streets, schools and businesses reopened, society returned to normal.
A third wave followed in January 1919, ending in the spring. This was lethal by any standard except the second wave, and one particular case would have an exceptional impact on history.
On April 3, 1919, during the Versailles Peace Conference, Woodrow Wilson collapsed. His sudden weakness and severe confusion halfway through that conference—widely commented upon—very possibly contributed to his abandoning his principles. The result was the disastrous peace treaty, which would later contribute to the start of World War II. Some historians have attributed Wilson’s confusion to a minor stroke. In fact, he had a 103 degree temperature, intense coughing fits, diarrhea and other serious symptoms. A stroke explains none of the symptoms. Influenza, which was then widespread in Paris and killed a young aide to Wilson, explains all of them—including his confusion. Experts would later agree that many patients afflicted by the pandemic influenza had cognitive or psychological symptoms. As an authoritative 1927 medical review concluded, “There is no doubt that the neuropsychiatric effects of influenza are profound...hardly second to its effect on the respiratory system.”
After that third wave, the 1918 virus did not go away, but it did lose its extraordinary lethality, partly because many human immune systems now recognized it and partly because it lost the ability to easily invade the lungs. No longer a bloodthirsty murderer, it evolved into a seasonal influenza.
Scientists and other experts are still asking questions about the virus and the devastation it caused, including why the second wave was so much more lethal than the first. Researchers aren’t certain, and some argue that the first wave was caused by an ordinary seasonal influenza virus that was different from the pandemic virus; but the evidence seems overwhelming that the pandemic virus had both a mild and virulent form, causing mild as well as severe spring outbreaks, and then, for reasons that remain unclear, the virulent form of the virus became more common in the fall.
Another question concerns who died. Even though the death toll was historic, most people who were infected by the pandemic virus survived; in the developed world, the overall mortality was about 2 percent. In the less developed world, mortality was worse. In Mexico, estimates of the dead range from 2.3 to 4 percent of the entire population. Much of Russia and Iran saw 7 percent of the population die. In the Fiji Islands 14 percent of the population died—in 16 days. One-third of the population of Labrador died. In small native villages in Alaska and Gambia, everyone died, probably because all got sick simultaneously and no one could provide care, could not even give people water, and perhaps because, with so much death around them, those who might have survived did not fight.
The age of the victims was also striking. Normally, elderly people account for the overwhelming number of influenza deaths; in 1918, that was reversed, with young adults killed in the highest numbers. This effect was heightened within certain subgroups. For instance, a Metropolitan Life Insurance Company study of people aged 25 to 45 found that 3.26 percent of all industrial workers and 6 percent of all coal miners died. Other studies found that for pregnant women, fatality rates ranged from 23 percent to 71 percent.
Why did so many young adults die? As it happens, young adults have the strongest immune systems, which attacked the virus with every weapon possible—including chemicals called cytokines and other microbe-fighting toxins—and the battlefield was the lung. These “cytokine storms” further damaged the patient’s own tissue. The destruction, according to the noted influenza expert Edwin Kilbourne, resembled nothing so much as the lesions from breathing poison gas.
**********
Seasonal influenza is bad enough. Over the past four decades it has killed 3,000 to 48,000 Americans annually, depending on the dominant virus strains in circulation, among other things. And more deadly possibilities loom.
In recent years, two different bird influenza viruses have been infecting people directly: the H5N1 strain has struck in many nations, while H7N9 is still limited to China (see “The Birth of a Killer”). All told, these two avian influenza viruses had killed 1,032 out of the 2,439 people infected as of this past July—a staggering mortality rate. Scientists say that both virus strains, so far, bind only to cells deep in the lung and do not pass from person to person. If either one acquires the ability to infect the upper respiratory tract, through mutation or by swapping genes with an existing human virus, a deadly pandemic is possible.
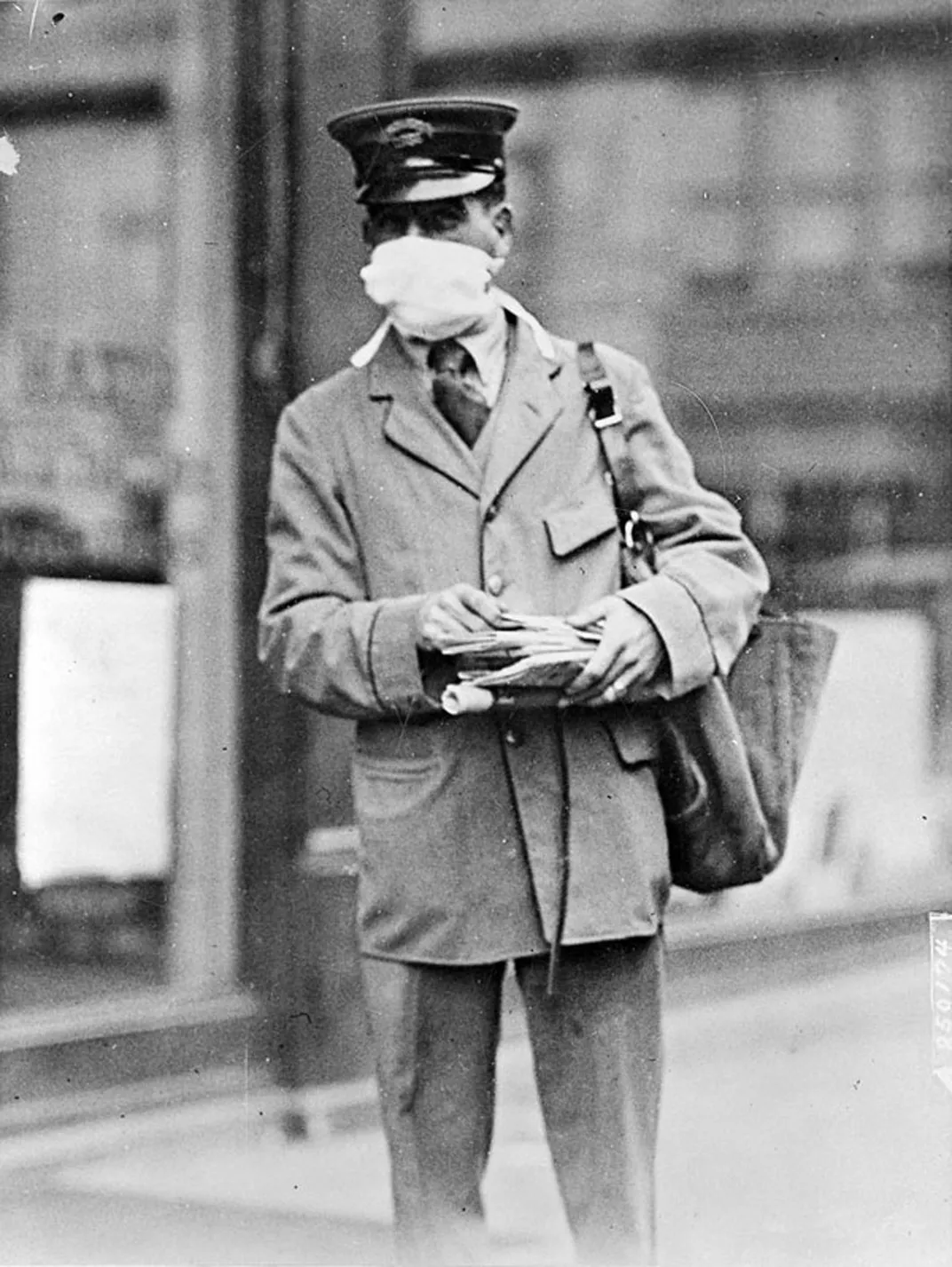
Prompted by the re-emergence of avian influenza, governments, NGOs and major businesses around the world have poured resources into preparing for a pandemic. Because of my history of the 1918 pandemic, The Great Influenza, I was asked to participate in some of those efforts.
Public health experts agree that the highest priority is to develop a “universal vaccine” that confers immunity against virtually all influenza viruses likely to infect humans (see “How to Stop a Lethal Virus”). Without such a vaccine, if a new pandemic virus surfaces, we will have to produce a vaccine specifically for it; doing so will take months and the vaccine may offer only marginal protection.
Another key step to improving pandemic readiness is to expand research on antiviral drugs; none is highly effective against influenza, and some strains have apparently acquired resistance to the antiviral drug Tamiflu.
The Great Influenza: The Story of the Deadliest Pandemic in History
Magisterial in its breadth of perspective and depth of research and now revised to reflect the growing danger of the avian flu, "The Great Influenza" is ultimately a tale of triumph amid tragedy, which provides us with a precise and sobering model as we confront the epidemics looming on our own horizon.
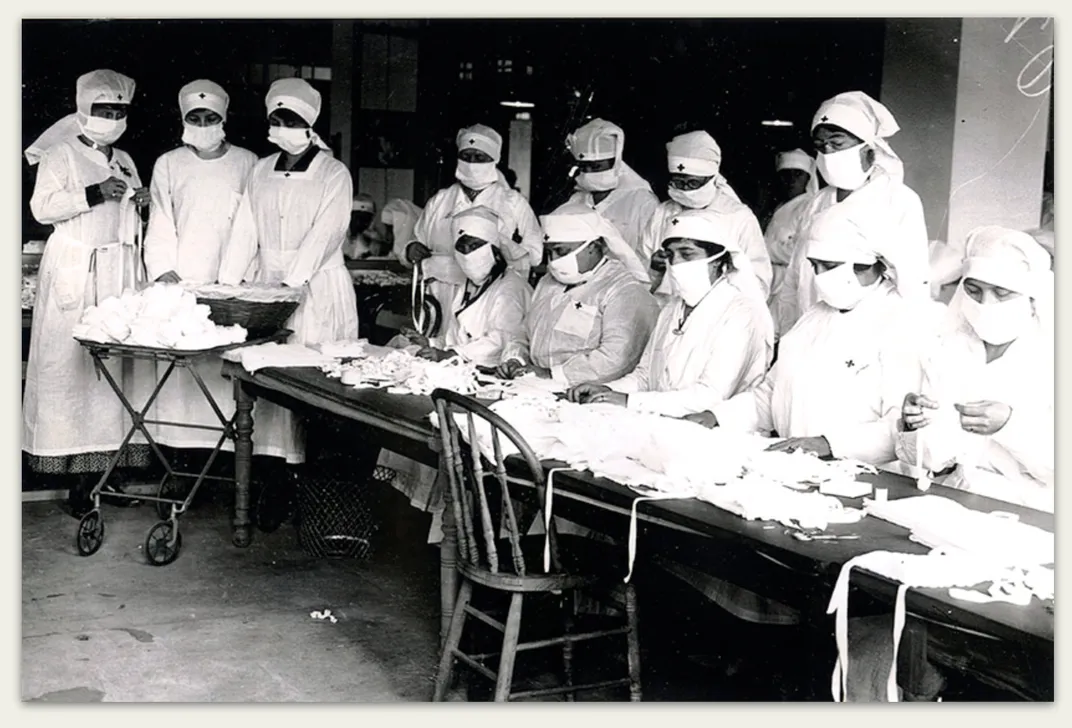
Then there are the less glamorous measures, known as nonpharmaceutical interventions: hand-washing, telecommuting, covering coughs, staying home when sick instead of going to work and, if the pandemic is severe enough, widespread school closings and possibly more extreme controls. The hope is that “layering” such actions one atop another will reduce the impact of an outbreak on public health and on resources in today’s just-in-time economy. But the effectiveness of such interventions will depend on public compliance, and the public will have to trust what it is being told.
That is why, in my view, the most important lesson from 1918 is to tell the truth. Though that idea is incorporated into every preparedness plan I know of, its actual implementation will depend on the character and leadership of the people in charge when a crisis erupts.
I recall participating in a pandemic “war game” in Los Angeles involving area public health officials. Before the exercise began, I gave a talk about what happened in 1918, how society broke down, and emphasized that to retain the public’s trust, authorities had to be candid. “You don’t manage the truth,” I said. “You tell the truth.” Everyone shook their heads in agreement.
Next, the people running the game revealed the day’s challenge to the participants: A severe pandemic influenza virus was spreading around the world. It had not officially reached California, but a suspected case—the severity of the symptoms made it seem so—had just surfaced in Los Angeles. The news media had learned of it and were demanding a press conference.
The participant with the first move was a top-ranking public health official. What did he do? He declined to hold a press conference, and instead just released a statement: More tests are required. The patient might not have pandemic influenza. There is no reason for concern.
I was stunned. This official had not actually told a lie, but he had deliberately minimized the danger; whether or not this particular patient had the disease, a pandemic was coming. The official’s unwillingness to answer questions from the press or even acknowledge the pandemic’s inevitability meant that citizens would look elsewhere for answers, and probably find a lot of bad ones. Instead of taking the lead in providing credible information he instantly fell behind the pace of events. He would find it almost impossible to get ahead of them again. He had, in short, shirked his duty to the public, risking countless lives.
And that was only a game.
A Note to our Readers
Smithsonian magazine participates in affiliate link advertising programs. If you purchase an item through these links, we receive a commission.