On the Trail of the West Nile Virus
Some scientists race to develop vaccines against the scourge while others probe the possible lingering effects of the mosquito-borne infection
During the dry hot summer of 2002, a telltale silence enveloped Chicagoand its suburbs like an insidious fog, too subtle to notice at first, too strange to ignore after a while. Residents in the affluent NorthShore communities and the well-to-do western suburbs noticed it. Folks in the modest suburban enclaves southwest of the city noticed it. Sooner or later, in a gradual and almost dreamlike way, people all around the city realized what was missing: the sound of crows. ~ BENNIE CASALINA and Yvonne O’Neill noticed it not long after they moved in June to Oak Lawn, a town of 55,000 people a few miles southwest of Chicago. Their one-story brick bungalow is set back from the tree-lined street and has a postage stamp of lawn in front and a small yard with a little flower bed out back. Bennie, a 71-year-old retired cement mason, is a sturdy, big-boned man with a bushy mustache and a fine mop of white hair over somewhat mournful eyes. He and Yvonne, a petite straight-talking woman, have been married for 13 years. It was Yvonne who first noticed the silence. “In the whole neighborhood, you never saw birds,” Yvonne said, recalling last summer. “The crows used to be out there cawing all the time, and then it got silent. You especially noticed the crows, because they’re usually so noisy.”
On August 9, a Friday, Bennie played golf with a neighbor, went home and developed a 103-degree temperature. The next day, still feverish, he began to see double. On Sunday, he awoke a little before 8 a.m., got out of bed and took a few steps toward the kitchen before collapsing onto the floor near a framed “Home Sweet Home” sampler. He was so weak he couldn’t pick himself up, couldn’t move, could barely call to his wife for help. By the time an ambulance took him to Advocate Christ Medical Center a few blocks away, he’d begun to “act crazy,” his wife said. He repeatedly tried to tear off his gown and had to be restrained. Then, suddenly, he lost the ability to speak, and the left side of his body became weak, almost paralyzed; he seemed “out of it,” Yvonne said. He was admitted to the hospital’s intensive care unit. His doctors weren’t sure what was wrong.
For weeks, Dr. Melvin Wichter had been seeing dead birds on the wooded streets around his home in Hinsdale, a suburb west of Chicago, and he, too, noticed that the familiar “cacophony of the crows,” as he put it, had disappeared. As he drove to work in Oak Lawn, he passed through an area that was once prairie and was now a concrete grid of expressways and residential areas interrupted by forest preserves and cemeteries. Without quite realizing it, he was driving through an environment that had the makings of an unprecedented epidemic.
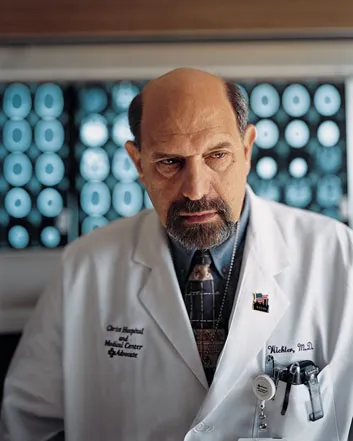
On Monday, August 12, Wichter met Bennie Casalina. The encounter was purely professional. Wichter is the president of ChristMedicalCenter’s medical staff and its former head of neurology, and late that summer he had been watching his service fill with people suffering from meningitis, an inflammation of the membrane covering the spinal cord and brain, or from encephalitis, an inflammation of the brain itself that can cause permanent neurological damage. “Encephalitis and meningitis are always uncommon in any hospital,” Wichter recalled one morning in his first-floor office. A Brooklyn native with a fringe of graying hair and a goatee, he looks something like an old beatnik. “Normally, we might consider encephalitis as a diagnosis maybe ten times a year, and maybe have two or three cases a year,” he went on. “To us, what was remarkable was we would come into work and see two or three cases a day. We were doing spinal taps like crazy.”
Wichter had a hunch it was something momentous, something spread by a mosquito. Roland Brilla, a neurology resident at the hospital, was skeptical. But as the test results trickled in from a state laboratory, it became clear that, as Wichter put it, “we were looking at history.”
What they were seeing was an encephalitis epidemic caused by the West Nile virus, an insect-borne, or arboviral, pathogen that was first found in humans decades ago in Africa and reached the United States in 1999. And 2002 turned out to be by far the worst year yet, with the Centers for Disease Control and Prevention (CDC) reporting 4,156 cases of illness and 284 fatalities caused by West Nile virus infection, compared with just 149 cases for the previous three years combined. Illinois led the nation in 2002 with 884 confirmed illnesses and 64 fatalities; some 600 of those cases occurred in CookCounty, which includes Chicago and many suburbs. Dr. William Paul, a deputy commissioner with Chicago’s Department of Public Health, watched the infection break out in the suburbs and then creep into the city, which recorded 227 cases of West Nile disease. “We knew the ingredients were there for a huge arboviral outbreak,” he said. “But I don’t think anybody predicted it would be this big in this part of the country.” Christ Medical Center, which had 56 cases, along with Evanston Northwestern Healthcare, which had 80, turned out to be two of the hottest spots in what would quietly become the largest epidemic of mosquito-borne encephalitis ever recorded in the Western Hemisphere.
Doctors told Yvonne O’Neill that Bennie wasn’t expected to recover. In early September, after Bennie had been hospitalized and essentially mute for three weeks, Yvonne pinned a copy of their wedding picture over his hospital bed. The next day, he opened his eyes, smiled and began talking again. He remained in the hospital another two weeks, and required extensive physical therapy and cognitive reconditioning after his release. He’s home now, but still struggling to regain his normal strength, and not yet able to get back on the golf course. “It’s hard to believe that this was caused by a little mosquito,” Bennie said while standing in his yard. “But all it takes is one, I guess.”
The West Nile virus was first detected in the United States in New York City in September 1999. I remember the autumn night that helicopters began spraying pesticides near our Brooklyn neighborhood. Like many New Yorkers, we tried to figure out how much of a threat this pathogen posed to ourselves, our children, our way of life. We tried to follow the city’s recommendations to use mosquito repellent. We dutifully removed receptacles of standing water in the backyard; it turns out that innocuous children’s toys, such as beach buckets or overturned plastic cars, hold enough water after it rains to breed mosquitoes. We also tried to avoid being outdoors after dusk, when the local arthropod air force was likeliest to bite, although we didn’t always resist the temptation to have dinner in the garden. I had read enough about the West Nile virus to know that the infection rate was quite low, and that the rate of serious neurological illness was extremely small. But I had a more visceral reaction the morning I went to fetch my 1-year-old son from his crib and was horrified to see that mosquitoes had gnawed on his legs. It’s a struggle to balance those reactions, intellectual and emotional, especially as new and disturbing information continues to pour in about a virus that has repeatedly surprised the experts.
By the spring of 2003, the virus had colonized 44 states and the District of Columbia. Last August, a woman in the Los Angeles area was hospitalized with West Nile virus infection, which she apparently acquired there, and California health officials expect the virus to make much more than a cameo appearance this year. The virus’s West Coast arrival was confirmed last fall, when a horse northwest of Seattle developed fever, anorexia and an unsteady gait because of West Nile infection. Researchers aren’t sure exactly how the virus spread across the nation, though migratory birds have likely contributed. The only states that haven’t reported an animal or human case of West Nile virus infection are Alaska, Hawaii, Oregon, Nevada, Utah and Arizona. But Grant (Roy) Campbell, a medical epidemiologist at the CDC’s Division of Vector-Borne Infectious Diseases in Fort Collins, Colorado, predicts that in 2003 “the map is likely to fill out in terms of the Western states.”
Researchers say the virus is astonishingly nimble. In the past year, health officials have documented that West Nile virus can be spread to the recipient of an organ transplant from an infected donor, from a pregnant mother to a fetus, by a blood transfusion from an infected person and possibly through breast milk. The blood-banking industry is working with the CDC, the Food and Drug Administration and the American Red Cross to begin screening the blood supply for West Nile as early as this year.
West Nile virus is known to infect more than 160 species of birds, even a partial list of which reads like the index of an Audubon field guide: chickadees, doves, eagles, finches, grackles, gulls, hawks, herons, kingfishers, owls, pelicans, sparrows, swans, turkeys, warblers, woodpeckers and wrens. Common birds such as sparrows and house finches also incubate the virus, and some researchers suggest that those birds may play an increasingly prominent role in urban epidemics.
Nor have other animals been spared. Veterinarians in Florida discovered last year that even alligators at a reptile farm had become infected (mosquitoes apparently can bite these thick-skinned reptiles on either their soft underbellies or around the eyes). Among the other mammals that the virus has been found to infect are bats, chipmunks, dogs, rabbits, reindeer and squirrels. West Nile virus infection last year afflicted some 14,000 horses, mostly in the Midwest.
Meanwhile, it remains unclear how serious a long-term threat the virus may be to human health—whether it will cause a lot of disease year after year, as some experts predict, or settle down and cause disease only rarely. Thomas Monath, chief scientific officer of Acambis—a British biopharmaceutical firm with a facility in Cambridge, Massachusetts, that hopes to begin testing a human West Nile vaccine in the United States this summer—said 2002’s heavy toll was probably only the beginning.Monath has impeccable credentials as an expert Cassandra in the field of arboviral disease. For 21 years he served at the CDC’s Division of Vector-Borne Infectious Diseases, and he literally wrote the book on one of the West Nile virus’s closest relatives, the St. Louis encephalitis virus. “The amplification of West Nile in 2003 could be worse than 2002,” he predicted, “and I think it could be a lot worse.”
It is part of American mythology that diseases spread by the bite of mosquitoes are scourges that happen somewhere else. Malaria continues to devastate Africa and tropical regions and claims one million to three million lives every year. Dengue, or “breakbone fever,” afflicts 50 million people worldwide and kills 24,000, mostly children. Yellow fever still plagues South America and Africa.
Those diseases are mostly strangers to our shores, but that wasn’t always the case. Yellow fever used to roar through New York, Philadelphia and New Orleans in the 18th and 19th centuries. American presidents fled the White House in summer partly to escape the seasonal yellow fever outbreaks that swept through Washington, D.C. But since the end of World War II, thanks to mosquito-control measures such as spraying pesticides and eliminating breeding sites, mosquito-borne diseases in the United States have largely been limited to outbreaks of generally rare viral illnesses that inflame brain tissue: St. Louis encephalitis (mostly in the South and Midwest), the eastern and western forms of equine encephalitis (which occasionally strikes humans) and La Crosse encephalitis (mostly in the Midwest).
The last major outbreak of mosquito-borne disease in the United States was the 1975 epidemic of St. Louis encephalitis, in which some 2,000 people were reported to have contracted the disease and about 170 to have died. Interestingly, the St. Louis virus epidemic struck many of the same Chicago-area neighborhoods that would be visited by the West Nile virus 27 years later.
“This community has been bitten before, so to speak,” said Wichter. Indeed, he took a job in 1977 at the Oak Lawn hospital because he had been intrigued by several cases of St. Louis encephalitis in the community. “I came here because of this St. Louis [encephalitis] experience,” he said with a laugh, “and of course we’ve never seen a case since. So I’ve been waiting for 27 years for something to happen!”
Illinois health officials had been on the lookout for West Nile since the spring of 2000, and they identified the first infected bird the next year. In 2002, said Linn Haramis, an entomologist with the Illinois Department of Public Health, authorities began bird surveillance on May 1 “and got our first dead bird on May 2.” By late July, people began showing up in emergency rooms complaining of fever, headache, muscle pain or weakness, stiff neck, sometimes with nausea or a rash; some had severe neurological problems, like mental confusion or an inability to walk. Because public health laboratories became overwhelmed with samples of blood and spinal fluid from suspected hospital cases, and also because the virus takes days to grow in the lab, physicians didn’t get conclusive test results back for two or three weeks. “It was very frustrating,” Wichter recalled.
Public concern exploded. In early July, the Illinois Department of Public Health was averaging 4,000 hits a week on the West Nile virus page of its Web site; by September, people seeking information were hitting the page 100,000 times a week. Local residents reported every dead crow. “Don’t send us any more birds!” the Chicago health department urged. Seemingly every animal case of West Nile—lapdog or wolf, sparrow or raptor—made the news. Chicago officials drained neglected residential swimming pools, a prime mosquito breeding site. Cemetery groundskeepers urged mourners not to leave vases at grave sites. City workers fanned out to place larvicide tablets in Chicago’s 210,000 sewer catch basins. Mosquito abatement trucks thrummed through the night spraying pesticides in the city and suburbs.
At the height of the outbreak, Wichter addressed the Oak Lawn Chamber of Commerce. Some 150 people crowded into the room to ask the questions that every community wants answered: How much of a risk does this virus pose to human health? What can we do to stop it? Wichter, who is also a professor of neurology at the University of Illinois School of Medicine, didn’t have all the answers. Although health officials recommend killing adult mosquitoes quickly when an arboviral epidemic is under way, Wichter, like many neurologists, is concerned about the potential harmful effects of pesticide use. “The issue of risk-benefit is not very clear,” he told the audience. “Some people will get West Nile fever, and fewer will get meningitis or encephalitis, and fewer still will have permanent disability. Only a minority of a minority will have any residual effects. So if you play that algorithm out, the numbers get really small. Is wholesale spraying justified with a disease of this benignity? You have dogs licking the grass and young children crawling through it. God knows what that will do to the [health] of our community.”
He later explained, “I could make the case for focused spraying in areas where there were large populations of mosquitoes. But I had the sense that the community wanted to see the trucks. Everyone knew someone who got sick, and they wanted to do something.”
“This was ground zero,” Tracey McNamara said, gesturing toward the flamingo pool at the Bronx Zoo. In an aviary just beyond the pond, terns and gulls whirled and banked. Cages holding the zoo’s raptors—a regal bald eagle, hulking vultures, a snowy owl—were right behind us. You could see the apartment buildings that crowd the streets just outside the zoo boundaries. You could hear the occasional cawing of a crow.
It was in the summer of 1999 that the zoo began receiving calls from alarmed residents who had been finding dead birds, especially crows, in the city. By August, dead crows were turning up on the zoo grounds. McNamara, who until recently served as the head of the zoo’s pathology department, sent dead crows to the laboratory of the New York State Department of Environmental Conservation, in Albany, for analysis; meanwhile, hundreds of dead crows were piling up in the state lab’s refrigerators. McNamara, worried that some unidentified pathogen was threatening the zoo’s animals, performed her own autopsies. The damage shocked her. She saw hearts ravaged by inflammation. In the brains of the birds, she saw pronounced “cuffs” of inflammation around blood vessels—the most severe brain damage she had seen in 18 years of animal postmortems.
Meanwhile, Deborah Asnis, director of the infectious disease division at Flushing Medical Center in Flushing, New York, had become alarmed by several strange cases of neurological illness at the community hospital, people with unexplained fever and headache, gastrointestinal distress, then confusion followed by muscle weakness. Most of the victims lived in a Queens neighborhood known as Whitestone, a few miles south of the Bronx Zoo across a finger of the East River. After a flurry of behind-the-scenes activity, New York City health officials and the CDC announced on September 3 that the cases represented an outbreak of St. Louis encephalitis. Officials were ecstatic to have identified the culprit. The city immediately began spraying.
But there was a problem. All the textbooks that McNamara skimmed that Labor Day weekend agreed that St. Louis encephalitis virus doesn’t kill birds. And birds were dying all over the place, including now at the zoo. The flamingos grew visibly ill, unable to hold up their heads, their elegant pink necks buckled in a desperate battle against gravity. A beloved bald eagle developed a head tremor. Acormorant swam in endless circles in the aviary pond. One by one, all those birds, and more, died.
“We lost the Guanay cormorant and a Chilean flamingo here, and the bald eagle over there,” McNamara recalled as we stood by the pool. She pulled her red parka tight, seemingly against the cold March wind but perhaps also against the memory of the virus that blew through the zoo’s bird population. On the morning of September 7, McNamara’s assistant brought her microscope slides bearing brain tissue from the dead flamingo, which looked just like tissue from the dead crows. “I saw the same encephalitis, and my heart just sank,” she said. “Because whatever it was, it was hot, it was bad, and I didn’t know what I had been exposed to.” On her way home that day, McNamara stopped to see a lawyer and drafted her will.
The coincidence was too much for McNamara to ignore. “The fact is,” she said, “I had a bunch of dead birds that had died of encephalitis at the same time that people had encephalitis.” McNamara—a strong personality, candid to the point of abrasion, but scientifically tenacious—refused to take St. Louis encephalitis for an answer, and the growing line of black-lidded specimen jars on a counter in her lab, each filled with the pickled tissue of the virus’s animal victims, gave her plenty of motivation. Before long, it wasn’t just birds. Arhinoceros developed a droopy lip, and a snow leopard became ill. Frantic for help, she sent tissue samples to the National Veterinary Services Laboratory in Ames, Iowa, which ruled out St. Louis encephalitis as well as other likely animal pathogens, and to the CDC’s Fort Collins lab, which declined to analyze her samples. Meanwhile, New York State health officials sent samples from human encephalitis victims to Ian Lipkin, an expert in neurological disorders of viral origin, then at the University of California at Irvine. At the end of September, Lipkin and the CDC (which did test human samples) concluded that the pathogen was not St. Louis encephalitis after all but West Nile virus, a pathogen not previously seen in the Western Hemisphere.
The virus derives its name from the West Nile District in Uganda, where the first human case was identified in 1937. It is found in Africa, the Middle East, Eastern Europe and Asia, where it causes sporadic outbreaks of human disease. Two main lineages of West Nile virus circulate in the world, and the one that reached North America is the more virulent; it’s nearly genetically identical to a strain that circulated in Israel in 1998. Whether it was carried here by an infected person or a bird or a mosquito, no one knows, and probably never will.
But the initial failure of U.S. health officials to quickly identify the pathogen exposed weaknesses in the nation’s ability to detect emerging infectious diseases that occur overseas and then jet to our shores; an even more recent example of how such a disease can spread is Severe Acute Respiratory Syndrome (SARS). Indeed, some experts believe that West Nile virus is more important as a wake-up call about the danger of other jet-setting microbes than a major public health threat. In that spirit, Dominic Travis, a veterinary epidemiologist at Chicago’s Lincoln Park Zoo, and McNamara, with CDC assistance, have organized a network of about 120 zoological parks in the United States to act as sentinels in monitoring the spread of West Nile among zoo animals—and perhaps to serve as an early-warning system for the arrival of other pathogens that affect humans and other animals. “The lessons to be learned from the West Nile outbreak in 1999 is that we received ample warning, at least six weeks before the first human cases,” McNamara said. But because it came from wild birds, she added, “the warning was ignored.”
“West Nile is extraordinarily good at adapting to this new environment,” said Lipkin, who is now director of the Jerome L. and Dawn Greene Infectious Disease Laboratory at ColumbiaUniversity. He takes in the Hudson River and seemingly half of New Jersey from his 18th-floor office. He has long studied bornaviruses, a largely obscure class of pathogens that may play a role in some mental illness. He tested the New York encephalitis samples with a variation of the method known as polymerase chain reaction, which analyzes nucleic acids, and identified the pathogen as West Nile virus, a type of flavivirus. Other flaviviruses include the ones that cause yellow fever and dengue.
Usually, an arbovirus is adapted to no more than a handful of mosquito species. By contrast, lab studies show that West Nile can take up housekeeping in at least 36 species of mosquito, making it one of the most versatile arboviruses ever. Michael Turell, an entomologist at the United States Army Medical Research Institute of Infectious Diseases at Fort Detrick, in Maryland, has shown that among the North American vectors are the northern house mosquito (Culex pipiens); the southern house mosquito (C. pipiens quinquefasciatus); a common pest mosquito in the West (C. tarsalis); and the recently arrived Asian tiger mosquito (Aedes albopictus), an aggressive daytime biter that may have played a significant role in last summer’s West Nile outbreak in Louisiana, which was known to strike about 330 people and kill 25. Human victims are essentially innocent bystanders who happen to get between mosquitoes and the virus’s original host, birds. The CDC currently estimates that less than 1 percent of people bitten by a mosquito infected with the West Nile virus will become severely ill.
To cause human disease, a mosquito must first bite an infected bird and pick up the virus. (Only female mosquitoes bite; they need blood protein to lay eggs.) The virus rides the slurp of blood into the insect’s gut, where it must infect the gut cells, replicate, pass through the gut wall, replicate again, and spread throughout the insect’s body until it reaches the salivary glands and the saliva itself. When the mosquito next bites bird, beast or person, it injects saliva, and the virus may then be passed along.
The complex transmission cycle depends on a great many factors. Consider temperature. If the temperature outdoors is 70 degrees Fahrenheit, Turell explained, it takes more than three weeks for West Nile virus to multiply throughout the body of a northern house mosquito, and only 10 percent of the mosquitoes will be able to transmit the virus. At 80 degrees F, the virus multiplies in two weeks, and 20 to 25 percent of the insects are infectious. But when the temperature goes to 90 degrees F, it takes only a week for the virus to multiply—and about 75 percent of the insects can transmit disease. It’s no coincidence that human outbreaks of West Nile virus disease typically begin in the late summer: the higher temperatures favor viral transmission, the number of infected birds is high and conditions are also prime for mosquito breeding.
West Nile virus causes unusually severe infections in crows and blue jays, according to one CDC-led study that measured the number of virus particles in the birds’ blood, or viremia. “I couldn’t believe the incredible viremias these birds cook up,” Monath, of Acambis, said of the study. “There’s no precedent for it. There were from a trillion to ten trillion viral particles per milliliter of blood”—that is, in an amount of blood equal to one-fifth of a teaspoon. “That’s beyond no precedent. That’s almost beyond belief. No selfrespecting bird can gin up a viremia higher than 100,000 particles with St. Louis encephalitis (SLE) virus. So some birds are almost a billion-fold more infectious with West Nile than with SLE.”
At first, scientists hoped that West Nile might fail to survive the North American winter. But the virus can lurk in dormant mosquitoes. “They go into storm sewers during the winter, go dormant, and just sit there resting,” said Stephen Higgs, a biologist at the University of Texas Medical Branch at Galveston. “The walls of some of these sewers are just furry with mosquitoes.” Researchers suspect that the virus might also survive in mosquito eggs that overwinter and hatch in the spring. There are already hints that West Nile has reached Mexico and the Dominican Republic, where the warm climate, researchers say, may lead to year-round disease activity rather than just seasonal outbreaks.
If, as most experts agree, West Nile has become established in North America, it may be a disaster for birds and other wildlife. Veterinarians at zoos in Los Angeles and San Diego were so alarmed by the threat of West Nile that they have used an experimental West Nile virus vaccine to protect their California condors. Zoo officials nationwide are deeply concerned about the virus. “We work really hard to be the ‘ark,’ ” said Travis of the Lincoln Park Zoo, “and this has the potential to blow through that.”
The future of human West Nile virus disease is trickier to assess. One possibility is that West Nile will follow the pattern of the St. Louis encephalitis virus, which causes only about two dozen cases of encephalitis annually. Scientists still don’t understand precisely why St. Louis encephalitis broke out in 1975 and has since faded. “We don’t know what West Nile is going to do in the future,” the CDC’s Roy Campbell said. “The best indicator is to look at what SLE has done. But in fact we are making a big leap of faith in saying it’s going to be like SLE.”
Some experts are unwilling to make that leap, including Anthony Marfin, a medical epidemiologist at the CDC’s Fort Collins branch. He sees parallels between West Nile virus and Japanese encephalitis virus, which causes between 30,000 and 50,000 cases of human encephalitis each year worldwide, but he said there wasn’t enough information yet to predict whether West Nile would become as common. Still, he speculated that eventually U.S. cases of West Nile disease may number in the hundreds each year, “with periodic explosions of thousands of cases.”
Federal, state and local officials began gearing up for the 2003 mosquito season as early as this past February. The city of Chicago started eliminating mosquito breeding sites and treating catch basins with insecticide this past May. “We can’t control the weather,” conceded city health official William Paul. “We can’t control bird migration patterns. What we can control is standing water in the urban environment.”
Still, the ability of health workers to detect arthropodborne disease has been seriously degraded over the past quarter-century. Since 1983, two National Academy of Sciences reports have warned of a looming shortage of medical entomologists and a steady decline of the infrastructure for surveillance of foreign pathogens. Both predictions have come true, according to Durland Fish, an entomologist at YaleUniversity. “We were better prepared to deal with this 30 years ago than we are now,” said Fish, who is developing satellite maps to analyze West Nile’s spread. “We don’t know how to predict human risk with this disease. We don’t know how to measure [its spread]. And even if we could, what would we do? We’d spray, and that’s a response that’s 50 years old!”
Some experts hold out hope for a vaccine. Monath said Acambis has manufactured its West Nile vaccine by splicing two of the virus’s outside proteins into a modified yellow fever vaccine, a strategy that has worked in a vaccine against dengue. Monath said that tests of the vaccine in monkeys have gone well.
Proving that a vaccine is really effective, however, won’t be easy. As the CDC’s Campbell pointed out, a scientifically valid clinical trial of the vaccine requires a large number of people exposed to the virus. “If we had thousands of cases a year, and we could predict where they were going to be, then yes, a vaccine could be very useful,” said Duane Gubler, director of the CDC’s Division of Vector-Borne Infectious Diseases. (The CDC is independently trying to develop a West Nile virus vaccine.) The problem is, Gubler added, no one can yet predict where West Nile will break out next.
There was an awkward moment when I first met Bennie and Yvonne at ChristMedicalCenter. We were seated around a conference table in Wichter’s office, and I asked Bennie if he felt back to normal after half a year. “Almost,” he said with a shrug, “but still a little foggy.” As he spoke, Yvonne was shaking her head. “His mind is not right, not back to normal,” she said with surprising bluntness, “just in terms of his thought processes and forgetfulness.”
The observation was anecdotal, but it echoed the results of a study by Denis Nash and colleagues at the New York City Department of Health, who found that only 37 percent of the people who developed West Nile meningitis or encephalitis in the original 1999 outbreak had fully recovered after 12 months. The finding raises questions about the longterm effects of West Nile infection, and whether there might be any more surprises in the clinical picture.
McNamara said something that might qualify as yet another whisper from the animal kingdom worth looking into. “We had a rhino that was symptomatic in September of 1999,” McNamara said. It recovered, but after it died some months later of an unrelated physical injury, McNamara’s department did a postmortem and were startled to find that the animal’s brain had remained inflamed, indicating ongoing damage from West Nile infection. Later, she examined two cranes that had previously been infected, but had shown no signs of illness. Their brains, too, bore signs of encephalitis. “So I thought, ‘Whoa, I have symptomatic and nonsymptomatic animals that have evidence of encephalitis,’ ” McNamara told me. “What does that mean for us?”
Clues, she went on, may be found in a 1983 study by Soviet scientists, who deliberately infected rhesus monkeys with several different strains of West Nile virus from Uganda, the Soviet Union and India. In many animals, viral infection persisted for nearly six months in the brain. Whether the infected animals developed encephalitis, or merely fevers, or no evident disease at all, autopsies found that the animal brains had undergone an “inflammatory degenerative process.” The findings are “really quite disconcerting,” said psychiatrist Mady Hornig of ColumbiaUniversity. She noted that the limbic region of the brains in these animals, which is associated with emotion and memory in humans, showed extensive damage, including atrophy and scarring. The implication is that people with West Nile infection who show no outward signs of illness could still harbor lingering brain infections that might ultimately produce neurodegenerative disease, an outcome previously reported with Japanese encephalitis, according to Robert Tesh, a virologist and epidemiologist at the University of Texas Medical Branch at Galveston. The number of people suffering from the long-term neurological effects of West Nile infection could be substantially larger than has been assumed. “We haven’t seen that yet in humans,” said Tesh, who has documented a similarly chronic, persistent West Nile brain infection in hamsters, “but it’s a possibility, and it should be studied.”
To be sure, medical researchers point out that the inflammation seen in animals could be medically irrelevant, like a scar that looks bad but doesn’t impair function at all. But researchers are only beginning to study the possible longterm health effects of viral infection. James Sejvar, a CDC physician, has studied 16 people in Louisiana infected by the West Nile virus. The most severely affected were three who developed a polio-like form of paralysis and had not improved after eight months. “It’s likely to be a persistent syndrome, so that’s kind of worrisome,” said Sejvar, who also said that some of the patients with meningitis and milder forms of encephalitis felt that they’d returned to normal after four months.
At a conference on West Nile virus sponsored by the CDC this past February in New Orleans, McNamara, who has a history of describing aspects of West Nile that people don’t necessarily want to hear, mentioned the long-term neurological damage she’d seen in infected birds that had never been obviously sick. “The room got very silent,” she recalled. As one health official later put it, “People are scared enough already.”
As the 2003 West Nile season draws near and I look out over all the water-friendly nooks and crannies in our backyard garden, each a potential incubator of mosquitoes, I realize that we know much more about West Nile now than in the fall of 1999, when the pesticide-spraying helicopters first flew overhead. I’m still reasonably persuaded that West Nile viral disease represents minimal risk to my family, but that risk is not totally in focus, and throughout the virus’s short sojourn in North America, birds and other animals have repeatedly tried to tell us something about the disease, and we haven’t always been particularly good listeners. While the scientists sort out the messages from the rhinos and monkeys and cranes, I’m going to be listening for the buzz of mosquitoes, and keep out of the line of fire.