Microbes: The Trillions of Creatures Governing Your Health
Scientists are just now beginning to recognize the importance of the vast community of microbes that dwells inside us
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/The-Body-Eclectic-microbes-631.jpg)
Of all the cases Barbara Warner has faced as a pediatrician specializing in newborns, the one that sticks hardest in her mind involved a couple who had been trying for years to have children. Finally, in 1997, the woman was pregnant. She was in her mid-40s. “This was her last chance,” says Warner. Then, too soon, she gave birth to twins. The first child died at two weeks of respiratory failure, at the time the most common killer of preterm babies.
A week later—it happened to be Thanksgiving Day—Warner folded down the blanket on the surviving twin, and even now she draws in her breath at the memory. The baby’s belly was reddened, shining and so swollen “you could have bounced a nickel off it.”
It was necrotizing enterocolitis, or NEC, little known outside neonatal intensive care units, but dreaded there as a sudden, fast-moving bacterial inflammation of the gut. On the operating table, a surgeon opened the baby boy’s abdomen and immediately closed it again. The intestinal tract from stomach to rectum was already dead. Warner, in tears, returned the child to die in the arms of his shattered parents.
“It’s 15 years later, and there’s nothing new,” Warner says bleakly as she moves among her tiny patients, each one covered in tubes and bathed in soft violet light, in a clear plastic incubator. NEC is still one of the leading killers of preterm babies. But that may soon change, thanks to a startling new way of looking at who we are and how we live.
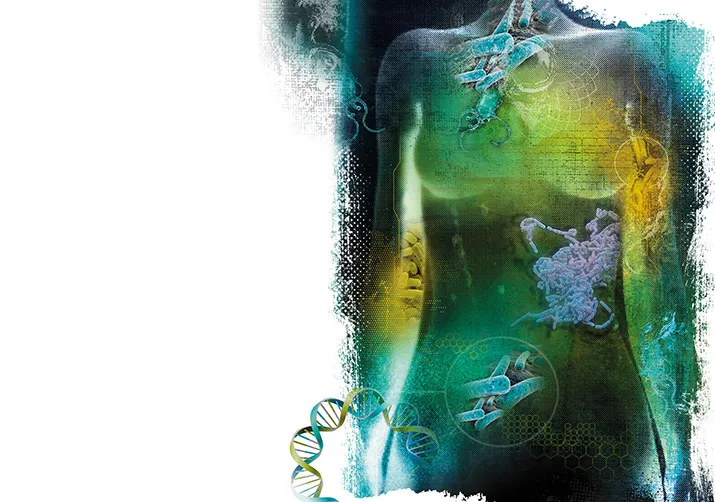
Over the past few years, advances in genetic technology have opened a window into the amazingly populous and powerful world of microbial life in and around the human body—the normal community of bacteria, fungi and viruses that makes up what scientists call the microbiome. It’s Big Science, involving vast international research partnerships, leading edge DNA sequencing technology and datasets on a scale to make supercomputers cringe. It also promises the biggest turnaround in medical thinking in 150 years, replacing the single-minded focus on microbes as the enemy with a broader view that they are also our essential allies.
The subject matter is both humble and intimate. In Warner’s neonatal care unit at St. Louis Children’s Hospital, researchers studying NEC have analyzed every diaper of almost every very low-weight baby delivered there over the past three years. They don’t expect to find a single pathogen, some killer virus or bacteria, the way medical discovery typically happened in the past. Instead, says Phillip Tarr, a Washington University pediatric gastroenterologist who collaborates with Warner, they want to understand the back-and-forth among hundreds of microbial types in the newborn’s gut—to recognize when things go out of balance. Their goal is to identify the precise changes that put a baby on track to developing NEC and, for the first time, give neonatal care units crucial advance warning.
A separate research group demonstrated early this year that secretions from certain beneficial microbes seem to relieve the deadly inflammation characteristic of NEC. So doctors may soon see into life-or-death processes that until now have been hidden, and take action to address them.
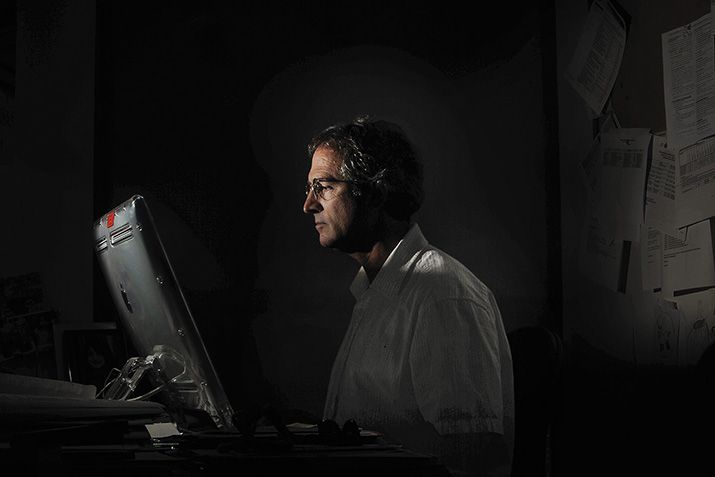
The new insights into NEC suggest why the microbiome suddenly seems so important to almost everything in the medical and biological worlds, even our understanding of what it means to be human. We tend to think that we are exclusively a product of our own cells, upwards of ten trillion of them. But the microbes we harbor add another 100 trillion cells into the mix. The creature we admire in the mirror every morning is thus about 10 percent human by cell count. By weight, the picture looks prettier (for once): Altogether an average adult’s commensal microbes weigh about three pounds, roughly as much as the human brain. And while our 21,000 or so human genes help make us who we are, our resident microbes possess another eight million or so genes, many of which collaborate behind the scenes handling food, tinkering with the immune system, turning human genes on and off, and otherwise helping us function. John Donne said “no man is an island,” and Jefferson Airplane said “He’s a peninsula,” but it now looks like he’s actually a metropolis.
***
The modern microbiome era started in the late 1990s, when David Relman, an infectious disease physician at Stanford University, decided to get a sample of the microbes in his own mouth. It’s a simple process: A dentist scrapes a sort of elongated Q-tip across the outer surface of a tooth, or the gums, or the inside of a cheek. These samples typically look like nothing at all. (“You have to have a lot of faith in the invisible,” one dentistry professor advises.)
Back then, such samples normally went to a laboratory to be grown in a petri dish for analysis, a good way to study those microbes that happen to be at home in a petri dish. Relman had the bold idea of adding DNA sequencing as a way of seeing every living thing. In the years since, the cost of sequencing has plunged and taking swab samples from various neighborhoods of the body for DNA analysis has become the standard practice of microbiome research.
In the laboratory, each Q-tip sample ends up in one of 96 little wells on a plastic collection plate smaller than a paperback book. A technologist then puts the plate on a sort of paint shaker, with a pebble and some detergent in each well to break open the cell walls, the first step in extracting the DNA. The resulting liquid gets drawn up by a pipetter—imagine a device with eight tiny turkey basters in a row—and transferred to wells in a series of eight more collection plates, each step taking the sample closer to pure DNA. The finished product then goes to the sequencer, a countertop device that looks about as impressive as an automated teller machine married to a bar refrigerator. But what it tells us about our own bodies is astonishing.
It’s not just that there are more than 1,000 possible microbial species in your mouth. The census, as it currently stands, also counts 150 behind your ear, 440 on the insides of your forearm and any of several thousand in your intestines. In fact, microbes inhabit almost every corner of the body, from belly button to birth canal, all told more than 10,000 species. Looked at in terms of the microbes they host, your mouth and your gut are more different than a hot spring and an ice cap, according to Rob Knight, a microbial ecologist at the University of Colorado. Even your left and right hands may have only 17 percent of their bacterial species in common, according to a 2010 study.
But the real news is that the microbial community makes a significant difference in how we live and even how we think and feel. Recent studies have linked changes in the microbiome to some of the most pressing medical problems of our time, including obesity, allergies, diabetes, bowel disorders and even psychiatric problems like autism, schizophrenia and depression. Just within the past year, for instance, researchers have found that:
•Infants exposed to antibiotics in the first six months of life are 22 percent more likely to be overweight as toddlers than unexposed infants, perhaps because antibiotics knock down essential microbes.
•A lack of normal gut microbes early in life disturbs the central nervous system in rodents, and may permanently alter serotonin levels in the adult brain. Scientists suspect that the same could hold for humans.
•Just giving enough food to starving children may not permanently fix their malnutrition unless they also have the “right” digestive micro-organisms, according to a study of kids in Malawi.
Researchers generally can’t say for sure if changes in the microbiome cause certain conditions, or merely occur as a consequence of those conditions. Even so, the intriguing correlations have stirred up intense scientific interest, particularly with the publication last June of the first results from the Human Microbiome Project, a $173 million effort by the National Institutes of Health. The aim of that project was to establish a normal profile of microbial life in 300 healthy individuals. For the medical community, it was like discovering a new organ within the human body—or more than that, a whole new operating system. Suddenly doctors had “another lever,” as an article in the American Journal of Epidemiology put it this January, “to pry open the proverbial black box” of human health and sickness.
***
The public has also embraced the microbiome, beginning a few years ago when researchers at Washington University noticed a curious fact about obesity: Fat mice have more of a bacterial group called Firmicutes in their guts and thin mice have more Bacteroidetes. Feed the mice the same diet, and the ones with more Firmicutes extract more calories and lay on more fat. When the same differences showed up in humans, it seemed to explain the common complaint of many overweight people that they get fat just smelling food their skinny friends gorge on with impunity.
Such studies have stirred up remarkable enthusiasm in a subject matter most people would once have dismissed as yucky, gross or worse. It’s as if people suddenly loved Gulliver’s Travels for the passage where Jonathan Swift depicts a scientifically inclined student trying to return human excrement to the foods from which it originated.
This past winter, two rival efforts invited microbiome enthusiasts to submit their own fecal, oral, genital or skin samples for microbial analysis, and each raised more than $300,000 from crowd-funded donations typically under $100 apiece. The first effort, managed by Rob Knight’s Colorado lab and called American Gut, emphasized participation by top scientists in the field. Prevention magazine ranked the project’s $99 “map of your very own gut bacteria ecosystem” among its top 10 foodie gifts for the holidays. (For romantics, the $189 “Microbes for Two” package included analysis of a stool sample for both you and your partner. Or your dog.)
Meanwhile, uBiome emphasized “citizen science,” with contributors formulating the hypotheses to be tested: “How does alcohol consumption change the microbiome?” or “What effect does a vegetarian diet have?” When Will Ludington, a co-founder, became a father in December, he began collecting daily fecal samples from his newborn son, Dylan, to answer his own question: “What is the succession of microbes colonizing the infant gut during the first year of life?”
Microbiome excitement has spread to venture capitalists, who have so far invested in at least four start-ups with the aim of developing new microbiome-focused drugs and diagnostic tools. At Second Genome outside of San Francisco (motto: “The most important genome in your body may not be your own”), chief executive Peter DiLaura has nearly $10 million in seed money and a plan to get to clinical testing within three years for drugs targeted at common conditions like ulcerative colitis, where the microbiome probably plays a causative role.
That timetable may seem optimistic, especially given that research on the first genome—that is, the human genome—has barely begun to produce the abundance of new therapies originally predicted. But at least in theory it ought to be easier to manipulate individual microbes. According to researchers in the field, several major drug companies working on diabetes and obesity now have research units dedicated to the microbiome. The big toothpaste and mouthwash companies are also investigating microbial methods to prevent tooth decay.
Even before such products come to market, merely being able to characterize a person’s microbiome may yield direct medical benefits. Research suggests that each of us has a distinct microbial fingerprint, with individual variation based on diet, family, medical history, ethnic or regional background, and a host of other factors. These differences seem to matter in ways both large and small. For instance, a person may have certain gut bacteria that alter the effect of a drug—even blocking a remedy as common as acetaminophen, the pain-relieving ingredient in Tylenol. At present, doctors sometimes fumble from one prescription to the next before finally hitting on the drug that helps a given patient. The ability to consult that patient’s microbiome profile could make it easier to get there on the first try.
Even so, some researchers worry that the microbiome movement may be promising too much too soon.
***
When a scientific team recently suggested that changes in gut bacteria could protect against stroke, Jonathan Eisen of the University of California at Davis lambasted them for “absurd, dangerous, self-serving claims that completely confuse the issue of correlation versus causation.” Eisen, a specialist in microbial genomics, now regularly presents “overselling the microbiome” awards on his blog. He says he doesn’t doubt the ultimate importance of the microbiome: “I believe the community of microbes that live in and on us is going to be shown to have major influences.” But believing that “is different from actually showing it, and showing it doesn’t mean that we have any idea what to do to treat it. There is danger here.”
For instance, probiotics, dietary supplements containing live bacteria, are generally harmless. Most contain the same microbes people have been consuming more or less forever. But exaggerated reports about beneficial microbes may lead people to regard the supplements as a cure-all, warns Richard Sharp, a bioethicist at the Cleveland Clinic. Manufacturers are careful not to claim specific health benefits because that would force them to undertake the kind of safety and effectiveness tests required for drugs. “But if somebody says they have a cure for everything,” says Rob Knight, “it’s probably a cure for nothing.” Still, U.S. probiotic sales were up 22 percent last year.
Researchers say they are only beginning to realize how subtle the interactions among our microbial species can be. They hope ultimately to develop probiotics that are correspondingly precise. But in the meantime, if the microbiome is like a symphony, then adding in current probiotics may be the equivalent of performing the piano solo with your elbows.
In certain rare circumstances, hitting the wrong notes may prove deadly. Administering probiotics before treatment seemed to make sense to the physicians in one study of severe acute pancreatitis, a bacterial inflammation of the pancreas. The theory, says the lead author, a Dutch gastroenterologist named Marc Besselink, was that a dose of beneficial microbes might crowd out dangerous microbes. That kind of “competitive exclusion” has worked well in some other conditions. But the pancreatitis patients receiving probiotics died more than twice as often as those who did not. The deaths occurred only in the most severe cases, where organ failure was already underway, and there was nothing to raise concern about the way most people use probiotics. But it was a wake-up call: The microbiome is a complicated system and we are only beginning to understand what happens when we tinker with it.
***
Blindly tinkering with the microbiome is, however, exactly what some researchers say we have been doing, willy-nilly, for more than 70 years, since the dawn of the antibiotic era. For Martin Blaser, a physician at New York University’s School of Medicine, one trend stands out: The typical child in the developed world now receives 10 to 20 courses of antibiotic treatment by the age of 18, often for conditions where these drugs do little or no good. “For two or three generations we’ve been under the illusion that there is no long-term cost to using antibiotics,” says Blaser, eyebrows rising over the tops of his wire-rimmed eyeglasses. It certainly hasn’t seemed like a cost for the child being treated, and only remotely for society at large (because excess use can lead to antibiotic resistance). But “you can’t have something this powerful,” says Blaser, “and change something as fundamental as our microbiome, at a critical time in development, and not have an effect.”
Though they have always known that antibiotics kill “good” bacteria as well as “bad,” doctors generally assumed the body’s microbial community was resilient enough to bounce back. But new studies show that the microbiome struggles to recover from repeated assaults, and may lose species permanently. Blaser suspects that diversity loss is cumulative, worsening from one generation to the next. He calls it “the disappearing microbiota hypothesis.” It’s like somebody played the piano solo with a two-by-four.
Along with the antibiotics, Blaser blames our obsession with cleanliness and antibacterial soaps and lotions. In addition, about 30 percent of American children are now born by Caesarean section. They start life without the microbiome they would normally have picked up passing through the mother’s birth canal, and some research suggests that this puts them at a disadvantage. Studies show that a diverse microbial community is essential to jump-start a baby’s immune system, establish a healthy digestive tract and even help shape the growing brain. Blaser doesn’t think it’s a coincidence that children now face an epidemic of medical disorders in all these areas, and that the surge in incidence tracks with an increase in Caesarean births and the introduction of powerful new antibiotics in the 1970s and ’80s.
“Here’s the point,” he says. “You have 10 or 12 diseases that are all going up dramatically, more or less in parallel—diabetes, obesity, asthma, food allergies, hay fever, eczema, celiac disease. They’re not going up 2 or 3 percent, they’re doubling and quadrupling. Each one may have a different cause. Or there could be one cause that’s providing the fuel, and my hypothesis is that it’s the disappearing microbiota.”
For Blaser, the decline of one “bad” bacterial species represents what’s happening to the entire microbiome. Helicobacter pylori, which lives in the human stomach, became notorious in the 1980s after scientists demonstrated that it is the essential precondition for almost all peptic ulcers and stomach cancers. The microbe was already on the decline from sanitary improvements and routine antibiotic use, but doctors then began directly targeting H. pylori in adults, incidentally meaning parents were less likely to pass the microbe on to their children. Today, while up to 100 percent of children in developing countries have Helicobacter, only about 6 percent of American kids do—and the latter is ostensibly a good thing.
“It’s good and it’s bad,” says Blaser. A study last year traced the human association with H. pylori back at least 116,000 years into our evolutionary history. “The idea that an organism that has been with us that long is disappearing in a century is striking,” says Blaser. “The good news is that it means less ulcers and less gastric cancer. The bad news is that it means more childhood-onset asthma and more esophageal reflux.” In certain circumstances, at certain times, Blaser argues, H. pylori may have protective effects not yet fully recognized.
The medical community has thus far resisted the rehabilitation of H. pylori. When Blaser first proposed that doctors would eventually find themselves reintroducing the species into American children, David Y. Graham, a gastroenterologist at the Baylor College of Medicine, replied in print, “The only good Helicobacter pylori is a dead Helicobacter pylori.” Of Blaser, he says, “He’s good at selling things.” Graham thinks Blaser is wrong to ascribe beneficial effects to H. pylori, and he worries Blaser’s message will dissuade people from seeking needed treatments.
Douglas Morgan, a Vanderbilt University gastroenterologist and epidemiologist, credits Blaser with pointing out the dual character of H. pylori. But the species may just look like the key player protecting against immune disorders because a simple medical test makes it the easiest to measure. Other microbes that rise and fall along with it could really drive the process, Morgan says.
Still, the attack on antibiotics doesn’t come casually. Blaser is a past president of the Infectious Diseases Society of America. Physicians who share his medical specialty depend utterly on antibiotics to treat patients suffering from pneumonia, heart valve infections and a deadly host of other disorders. But infectious disease specialists also see the cost being paid for their reliance on antibiotics, says Relman, a fellow microbiome researcher, physician and current president of the Infectious Diseases Society. These doctors have become dismayingly accustomed to saving patients’ lives, he says, only to see them go home and develop a crippling and sometimes fatal case of Clostridium difficile. “C. diff.,” as it’s known, is an intestinal infection with chronic diarrhea, and incidence in the United States has more than doubled since 2000. The problem almost always results from antibiotic use that has destroyed the normal population of microbes, clearing the way for just one, C. difficile, to dominate. So far, the only conventional remedy is another antibiotic.
***
In a procedure room at Rhode Island Hospital in Providence, a gastroenterologist named Colleen Kelly sprays a little air freshener, says “Breathe through your mouth” and then opens a plastic container of donor material, delivered fresh this morning by a relative of today’s patient. Kelly mixes it into a half liter of saline solution, then shakes it up like a bartender mixing a mai tai. She draws the liquid off into a half-dozen syringes the size of handheld bicycle pumps, and then it’s time to wheel in the patient.
The idea of fecal transplants is not new. Veterinarians have long used them to treat livestock with digestive troubles. Human cases in the United States, though rare, date back at least to the 1950s. But the procedure has become more common recently because it seems to cure C. diff. infection. Janet O’Leary, a medical imaging technologist in Massachusetts, went to Kelly for the procedure last October. “I told my boyfriend what I was going to do,” she recalls, “and he said, ‘I absolutely don’t believe it. You’re making this up.’”
Her personal physician felt almost as horrified. “It’s considered fringe, and this is how medicine in America works,” O’Leary says. “It’s not a drug. Nobody’s making money off it. Yet. It’s not being pushed by a dozen companies. It’s just a natural way to get the normal flora back in your gut. My response is that there is no ‘yuck factor’ for people who are this sick.”
O’Leary had come down with C. diff. after a vacation trip on which she used a powerful antibiotic for turista. Back home, her doctor prescribed another round of the same antibiotic, and the problem just got worse. A different antibiotic followed, and then repeated courses of a third antibiotic. It got so bad O’Leary couldn’t go to work at her hospital. She became a patient instead. “This wasn’t getting better. It was pretty scary, and the doctors were saying they might try another round of antibiotics, or I might lose part of my colon.”
Instead, O’Leary contacted Kelly, one of a few dozen gastroenterologists around the country now performing fecal transplants. The donor is usually a family member, says Kelly, and must be screened beforehand to ensure against introducing known pathogens. The procedure itself is a basic colonoscopy. But on the way back out, Kelly screws those bicycle-pump syringes into the instrument panel of her colonoscope and injects the contents at various points in the colon. The phrase is to “seed them through,” planting a healthy microbiome like a landscaper installing a new garden.
Of 94 C. diff. patients she has treated, Kelly says, all but three have overcome the infection. She’s now participating in a National Institutes of Health study to test the effectiveness of the procedure against a placebo in a double-blind clinical trial. She also foresees a time when a carefully designed probiotic manufactured in a laboratory will obviate the need for a human donor. One researcher has already begun testing an experimental version. It’s named RePOOPulate.
For the rest of us, the idea of fecal transplants, or of ulcer-causing bacteria as our sometime-friends, or of babies being anointed into humanity at birth by their mother’s microbiome, will no doubt continue to sound a little gross for a while to come. But here’s a way to put that in perspective: Vaccination also sounded gross when Edward Jenner figured out in the 1790s that inoculating people with pus from a cow could protect them from smallpox. And it was gross in 1928 when Alexander Fleming began the process of turning a moldy growth into penicillin. But vaccines and antibiotics would go on, in time, to become the most important discoveries in the history of medicine, and they now routinely protect billions of people from disease.
Coming to understand our microbes not as enemies, but as intimate partners could change our lives at least as dramatically, with time and proper testing. Asked recently about the prospects for microbiome research, one scientist not directly involved put it this way: “To make an analogy, we’re roughly a year after Fleming found penicillin.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/richard-conniff-240.jpg)

/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/richard-conniff-240.jpg)