Why Black, Indigenous and Other People of Color Experience Greater Harm During the Pandemic
Scholars take a deep dive into how structural racism intersects with public health
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/e7/0a/e70a0753-cb75-467a-a92c-7b8fb800a840/gettyimages-1228122152.jpg)
History, as nearly no one seems to know, is not merely something to be read. And it does not refer merely, or even principally, to the past. On the contrary, the great force of history comes from the fact that we carry it within us, are unconsciously controlled by it in many ways, and history is literally present in all that we do. It could scarcely be otherwise, since it is to history that we owe our frames of reference, our identities, and our aspirations. —James Baldwin, “Unnameable Objects, Unspeakable Crimes,” 1966
Structural racism is inextricably intertwined with the political and legal systems in the United States, a legacy that predates the country’s founding, through the genocide of Indigenous populations and the kidnapping and selling of millions of Africans into slavery.
Preeminent public health scholar and former president of the American Public Health Association Camara Jones defines structural racism as “a system of structuring opportunity and assigning value based on the social interpretation of how one looks (which is what we call ‘race’), that unfairly disadvantages some individuals and communities, unfairly advantages other individuals and communities, and saps the strength of the whole society through the waste of human resources.”
This system directly and indirectly impacts public health and the wellbeing of populations and results in stark racial differences across various health outcomes. It underscores that deep racial health inequities are not a result of the dispelled theory of biological “race,” but are driven by structural racism—the policies, practices and norms that create and uphold racial superiority and inferiority.
Today’s compounded public health crises of COVID-19 and police violence have disproportionately impacted Black, Indigenous and People of Color (BIPOC) and elevated the global discourse around structural racism. The recent police killings of George Floyd and Breonna Taylor, and the recent police shooting of Jacob Blake clearly reflect historical and contemporary manifestations of structural racism in the form of police violence.
This same structural racism is also equally responsible for the elevated rates of COVID-19 infection and death among Black, Indigenous and Latinx people. This particular moment is a blatant reminder of just how embedded structural racism is in American society, both historically and in the present.
The work of dismantling this system requires collective power. The responsibility to upend it lies with all of us.
Structural Racism as a Public Health Issue
Hundreds of years of unjust and racist policies and practices in the United States continue to impact where people may live and work, the air they may breathe, the quality of their education and their access to healthcare. All of this affects health and wellbeing. Scholars have produced a large body of research examining the health impacts of structural racism. Even the most prominent medical and public health professional associations, including the American Medical Association, the American Academy of Pediatrics, and the American Public Health Association, have released public statements calling for urgent recognition of and attention toward the health impacts of structural racism.
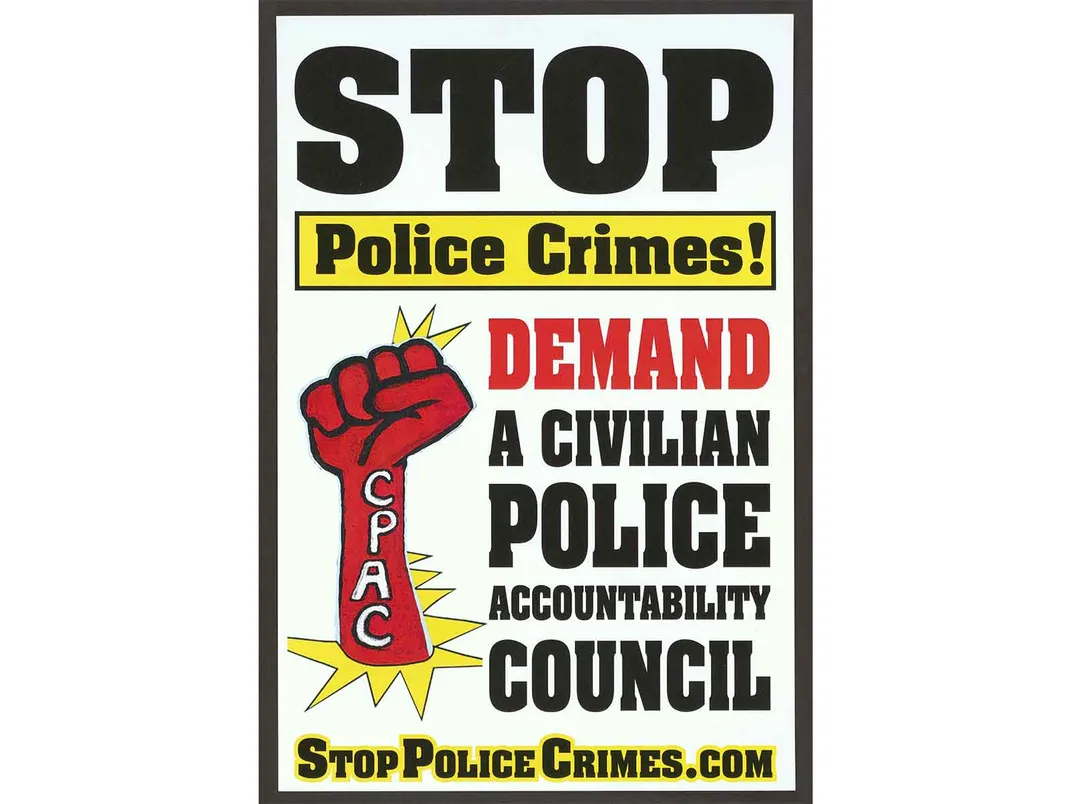
One of the many manifestations of structural racism that still needs to be addressed as an urgent public health crisis is police violence. Developed in large part from the system of slave patrols dating back to the 1700s, the institution of policing continues to be a source of violence against Black communities, in particular, and communities of color more broadly.
Long before the recent headlined police killings, the field of public health officially recognized police violence as a public health issue, and scholars have documented its devastating impact on the health of communities of color. For example, researchers examining premature mortality due to police violence found that upwards of about 55,000 years of life lost (a measure of premature mortality) were due to killings by police—a burden similar in magnitude to maternal deaths and greater than unintentional firearm injuries. Most significantly, despite making up only 38.5 percent of the U.S. population, BIPOC comprised 51.5 percent of these premature deaths at the hands of police violence.

These same communities are also more likely to become sicker and die from COVID-19. Racist systems and structures that long precede the pandemic impact BIPOC’s increased risk of exposure to and complications from SARS-CoV-2, the virus causing COVID-19.
These systems and structures create disparate rates of heightened chronic health conditions, poor working environments and denser and crowded housing. These persistent inequities can be traced back to the Jim Crow era (1877–1954), when the progress that Black communities made during the brief Reconstruction era was intentionally upended through state-driven segregation in healthcare, job opportunities and housing.
Long after the end of Jim Crow, institutions continue to uphold racist practices that still leave BIPOC in this country with subpar resources across all these sectors. As a consequence of these inequitable policies, Black and Latinx people are three times more likely to be infected with SARS-CoV-2 than white people and two times more likely to die from it. Compared with white people, American Indian/Alaska Native individuals are approximately five times as likely to be hospitalized for COVID-19, and at one point the Navajo nation had a higher infection rate than all of New York state.
Structural racism also lives at the intersection of these crises. We see this in the ways policing further exacerbates the disproportionate impact of COVID-19 on BIPOC communities. Chronic stress from being exposed to over-policing can result in cumulative wear and tear of the body.
This physiological deterioration can lead to adverse health outcomes such as hypertension, that serve as underlying risk factors for COVID-19 complications. Furthermore, the very measures intended to protect people from COVID-19—physical distancing and public mask-wearing—create heightened opportunities for law enforcement to further brutalize and racially profile BIPOC. Consequently, communities of color are left to choose between the risk of acquiring COVID-19 and the risk of experiencing police violence—both of which can have lethal consequences.

Failed Responses to Public Health Crises
The responses to both of these crises demonstrate the devaluation of BIPOC lives. Our country’s COVID-19 response has largely failed communities of color. Since the start of the pandemic, we have heard reports of countless BIPOC with COVID-19 symptoms being turned away from obtaining testing.
As the pandemic ravages the country, people of color face testing shortages, with few testing centers available in their communities. Additionally, the federal stimulus package, meant to provide economic relief for families experiencing financial strain due to the pandemic, excluded many vulnerable communities. Most notably, undocumented people, many of whom are Latinx essential workers, were ineligible.
And despite the well-documented, devastating impact of this pandemic on BIPOC populations, many state governments dismissed public health warnings and began reopening. This woefully inadequate state response is reminiscent of the countless times BIPOC in this country have been historically harmed by medicine and public health.
The public health response of the 1918 influenza pandemic is particularly emblematic of the systemic negligence of Black lives. In the midst of this pandemic, many Black people fled the segregated Jim Crow South for a promise of better life in Northern cities where they were instead met with prejudice, violence and segregationist policies. Public health officials and medical workers blamed Southern Black migrants for spreading the flu. The social conditions many of these migrants were subjected to as a result of segregationist housing practices—including squalid housing conditions and overcrowding—were cited as pathologies responsible for the outbreak.
As a 1917 Chicago Daily Tribune article excerpt highlights, these migrants were seen as culpable for their own conditions: “compelled to live crowded in dark and insanitary rooms.” Consequently, Black influenza patients received substandard care in segregated and under-resourced hospitals. As Black deaths mounted, institutional racism persisted. For example, white sanitation employees in Baltimore refused to dig graves for Black influenza victims after the city’s only Black cemetery was filled to capacity. As with the 1918 flu pandemic, today’s COVID-19 pandemic exposes the politics of BIPOC disposability.
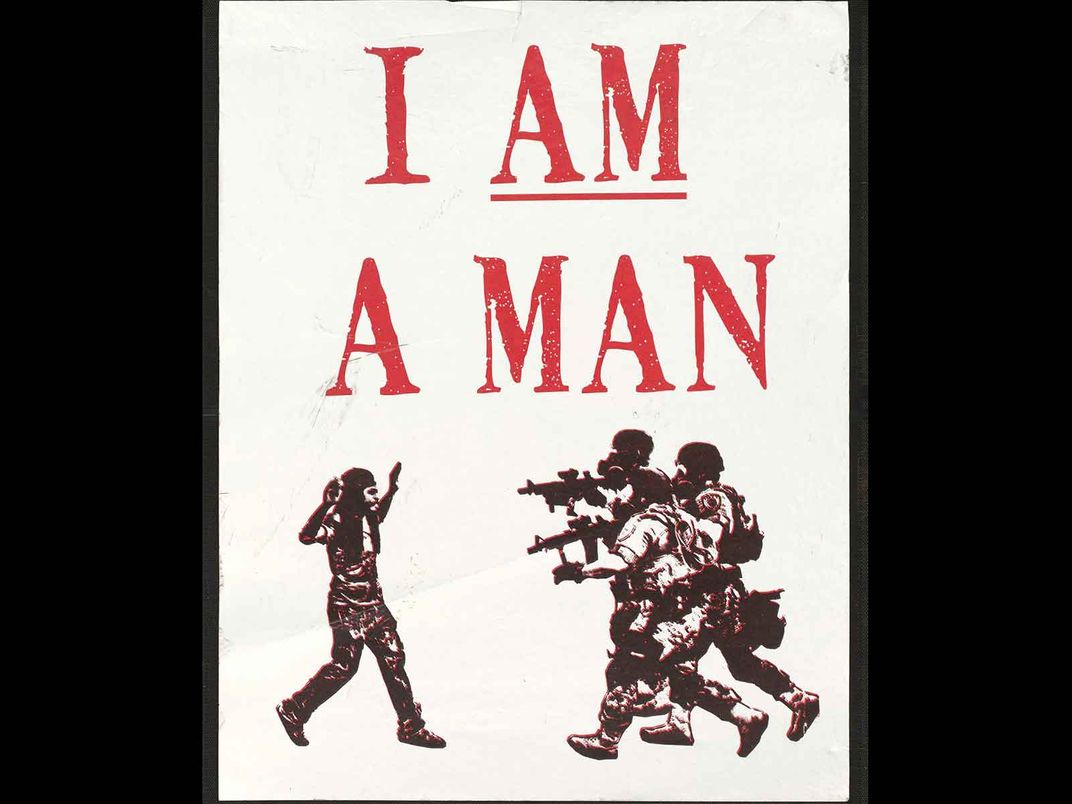
If our nation’s response to COVID-19 is wholly inadequate, then the government response to the protests against police violence is abysmal. In the wake of the violent police killing of George Floyd, a 46-year-old Black man in Minneapolis, many people took to the streets, affirming that Black Lives Matter and calling for systemic transformation of policing.
More than 1,200 health professionals and community stakeholders wrote an open letter in support of protests as vital to dismantling white supremacy, “a lethal public health issue that predates and contributes to COVID-19.” Despite this support, calls for justice have been met with institutional ridicule and dismissal.
Without any conclusive evidence, politicians, news outlets, and individuals on social media platforms blamed protesters for increased COVID-19 cases. Demonstrators were deemed hostile and met with militant law enforcement tactics, including tear-gassing, kettling and mass jailings; increasing their risk for COVID-19.
Institutional forces have long sought to control and dismiss protests against structural racism. Medicine and public health are far from exempt. In “The Protest Psychosis: How Schizophrenia Became a Black Disease,” psychiatrist and historian Jonathan Metzl explores the overdiagnosis of schizophrenia among Black men in the 1960s and 1970s. His study reflects on the racialized diagnostic language of “hostility” and “aggression” in the DSM-II (the diagnostic manual for psychiatry published in 1968). Metzl analyzes medical charts from a large psychiatric hospital in Michigan, revealing how psychiatric symptoms were applied to Black male patients aligned with protest movements of the time, such as the Black Panthers and Black Power movement.
This country has never affirmed the right to protest in response to structural racism because it has yet to reckon with what calls for such protest. Particularly when Black people practice their right to protest, our country has pathologized and retaliated with a callousness that again exposes its devaluation of Black life. Time and time again we are reminded whose lives are valued and whose are deemed dispensable in this country.

A Way Forward: Toward Dismantling Structural Racism
Both police violence and COVID-19 reveal the inextricable links across systems rooted in structural racism that disparately harm BIPOC. Emblematic of this are the autopsy results revealing that George Floyd was positive for COVID-19. Making instrumental strides towards addressing both crises requires dismantling structural racism.
Building on centuries of antiracist efforts, communities continue to mobilize across the country. In response to this historic moment, we see calls for and action towards police divestment and reinvestment in BIPOC communities. We see the establishment of bail funds for demonstrators. We see the formation of mutual aid efforts for COVID-19 relief. We see local organizing of COVID-19 testing sites.
Shaping a brighter future and imagining a nation anew require a confrontation of the histories of this nation—the legacies of settler colonialism, genocide and enslavement—their embodiment ever present in the here and now. This moment refocuses the struggle for health equity as a struggle against racism, requiring intersectional and community-led solutions across systems. It challenges us as a nation to reimagine a society that no longer disavows and devalues BIPOC lives but truly ensures health and wellbeing for all.
Mahader Tamene is a PhD student in the Division of Epidemiology at UC Berkeley's School of Public Health. A public health scholar and practitioner dedicated to facilitating health and justice for underserved populations globally, her work focuses on maternal and child mental health disparities, particularly community-based interventions that address the structural forces driving these disparities. Tamene has worked in community health education, health research, program implementation and evaluation both domestically and abroad. She holds an MSc in global health and population from the Harvard T.H. Chan School of Public Health and a BA in public policy and African/African-American studies from the University of Chicago.
Elleni Hailu is a PhD student in Epidemiology at UC Berkeley School of Public Health. Her research interests address the ways in which place-based markers of structural racism (for example, mass incarceration) are biologically embedded across the life course to influence racial inequities in cardiovascular and adverse maternal health outcomes.
Dr. Rachel L. Berkowitz is a Postdoctoral Research Fellow in Health Equity & Implementation Science with the University of California, Berkeley, and the Sutter Health Center for Health Systems Research. Her work focuses on understanding and addressing how systems, structures, and places create and perpetuate health inequities. Her current projects involve assessing the ways in which neighborhood contexts influence and drive racial inequities in health outcomes (with a particular focus on birth outcomes and maternal outcomes), understanding how social determinants of health affect patient wellbeing, and examining the impacts of changes resulting from the COVID-19 pandemic on the experiences and outcomes of patients and providers.
Xing Gao is a doctoral student in the Department of Epidemiology at University of California, Berkeley. Her research interests center around neighborhood context, geospatial manifestations of structural racism, and the wellbeing of communities of color.