The Woman Who Revealed the Missing Link Between Viruses and Cancer
Today, vaccinating against cervical cancer is routine. But before Sarah Stewart, scientists dismissed the idea of a cancer-preventing vaccine as ludicrous
:focal(359x142:360x143)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/74/7a/747ad874-b593-4ae5-b1cd-eecefdc4f806/sarah_elizabeth_stewart.jpg)
If you’re an adolescent girl getting your annual checkup in the United States, your doctor will almost certainly double-check that you’ve gotten the HPV vaccine, otherwise known as Gardasil. The vaccine, which is 100 percent effective against certain strains of the human papillomavirus, is a no-brainer. Today it’s just one of the standard battery of vaccines recommended for preteen boys and girls across the country. But when it was first approved by the Food and Drug Administration in 2006, it was revolutionary.
Until the 1960s, scientists considered the idea of a cancer-causing virus to be preposterous. At the same time, more than 8,000 women a year were dying of cervical cancer, and researchers couldn’t figure out what was causing it. It was only in 1976 that a virologist named Harald zur Hausen identified the human papillomavirus, one of the first viruses known to lead to human cancer. From 1975 to 2014, deaths from cervical cancer dropped by 50 percent. In the future, widespread vaccination could lower cases of cervical cancer by as much as 90 percent, according to the National Cancer Institute.
The rise of vaccines like Gardasil represents a major sea change in how researchers viewed cancer development. And yet one of its major players is nearly unknown. Way back in the 1950s, bacterialologist Sarah Stewart pioneered the concept that viruses could lead to cancer—and was almost thrown out of the scientific community for her heretical ideas. In 1957 she demonstrated that the polyoma virus could cause cancerous tumors in mice, a finding that fundamentally transformed how researchers treated and prevented cancer. Stewart didn’t even have cancer on her radar when she started her scientific career—but once she entered oncology, the field would never be the same.
Stewart was born on August 16, 1906 in the state of Jalisco, Mexico, one of four children. Her father George, an American mining engineer who owned gold and silver mines in the region, met and married her mother, Maria Andrade, in the state. We know little else about her parents and her childhood. But in 1911, the family’s life in Mexico was interrupted by local and national unrest in the wake of President Porfirio Diaz’s exile to France and the beginning of the Mexican Revolution. The Mexican government ordered Stewart and her family to leave, and they fled to Cottage Grove, Oregon, where George owned land.
When Stewart was in high school, the family moved to New Mexico. Stewart ended up going to college at New Mexico State University in Las Cruces and majoring in home economics. It was the best major open to women at the time, and it featured all the same courses as a general science degree aimed at men. “We took chemistry and all other courses, along with everybody else,” Stewart said in a 1964 interview with historian Wyndham Miles. “The girls took the very same courses the fellows did.” By the time she graduated in 1927, she had managed to earn two bachelor’s degrees in home economics and general science.
After graduation, Stewart taught home economics at a small high school in Tatum, New Mexico. It was the only option available to her—but it wasn’t enough. “After half a year of that I … applied for fellowships, just picking places at random over the country,” she later recalled. She soon got a bite from the University of Massachusetts, where she accepted a fellowship offer in their graduate program and earned a master’s degree in microbiology in 1930.
That same year she took a position as the first bacteriologist at the Colorado Experimental Station at Fort Collins, an agricultural research center where she worked on nitrogen-fixing bacteria for better crop yield. “I worked there for three years,” she said, “and it was in soil bacteriology, which I wasn’t interested in, so then I decided to get my PhD.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/45/83/458312c9-bce8-4e82-93a5-a324fb44dc24/stewart_sarah_elizabeth_cw.jpg)
She began doctoral work at the University of Colorado School of Medicine in Denver in 1933. But two years into her doctoral studies, Stewart took an unpaid position at the National Institutes of Health as a research assistant to Ida Bengtson, the first woman scientist to work at the Public Health Service. Eventually Stewart took over Bengtson’s work in anaerobes, organisms that survive without oxygen. Gangrene, an anaerobic infection, was common in war wounds, and Stewart helped developed toxoids for gangrene treatment and immunization that would later be used in World War II.
Stewart finished her PhD at the University of Chicago in 1939 while on assignment for the NIH. At this point she again became disinterested in her work on anaerobes and toxoids. She left the NIH in 1944 with the intention of earning a medical degree and switching over to cancer research. For some reason, she was seized at this time by the conviction that there was a connection between viruses and cancer. “My feelings have always been that certainly certain cancers are virus-induced,” she said. But she had little idea how controversial her ideas would be. “There was a tremendous feeling against viruses and cancer, which I never, never had realized.”
The first hint that it was going to be a long uphill battle came when she submitted a proposal to the NIH asking for support to study tumors and viral etiology. Both the NIH and the National Cancer Institute (NCI) refused, saying that she was not qualified to work on human research—she had never worked on sciences that directly involved mammals, much less humans—and that her proposal was “dubious.” To gain the necessary experience and bolster her legitimacy, Stewart decided to work toward a medical degree.
There was just one problem: In 1944, women weren’t yet allowed to enroll as full students in most American medical schools. By a stroke of luck, Stewart found a workaround. She accepted a post at Georgetown University Medical School as an instructor in bacteriology, which allowed her to take medical courses for free, even if she was not considered a full student. In 1947, the medical school began to accept women, and she formally enrolled. In 1949, at the age of 43, Stewart became the first woman to earn a Georgetown medical degree.
Stewart returned to the NIH but was still denied the option to study cancer. Instead, she took a temporary position in a hospital in Staten Island where she was assigned to gynecology. Alan Rabson, a researcher and later deputy director at NCI, recalled in a 1987 interview that when Stewart finished her stint in Staten Island, “she came back and said now she was ready to prove that cancer [was] caused by viruses. The director said not around here you won’t. So they wouldn’t let her come back.” But Stewart was appointed medical director in the United States Public Health Service Commissioned Corps and took up a position at the NCI in Baltimore, where she finally had the professional leverage and resources to begin her work in earnest.
At the time, oncologists weren’t ready to consider that viruses could cause cancer in humans. In an interview with Smithsonian.com, Gregory Morgan, a historian and philosopher of science at the Stevens Institute of Technology, gives two reasons for this. “There were some people who thought that the environment causes cancer and various chemicals could cause cancer,” he explains. “The other thing that people expected was if cancer had [a] viral cause, then you’d expect it to have similar patterns to infectious diseases. So if someone had cancer then they in theory would be able to transfer it to somebody else. And those patterns weren’t really seen.”
Stewart’s search for a viral basis for cancer wasn’t unprecedented. In 1911, virologist Peyton Rous discovered the Rous sarcoma virus, which he concluded could transmit cancer in chickens. In 1933, Richard Shope, a physician and virologist, discovered the Shope papilloma virus, which caused keratinous carcinomas in rabbits, and three years later, biologist John Bittner demonstrated that the mouse mammary tumor virus could be transmitted from a mother mouse to her young through her milk. But it was Ludwig Gross’s work on leukemia in mice in the 1950s that would lead to the first major breakthrough in the virus-cancer link—and it was that work that Stewart took up when she moved to the NCI in 1951.
Gross, originally an immunologist, had also been struggling to gain respect for his research. While working in the basement of the Veterans Administration Hospital in the Bronx in 1951, he discovered a murine leukemia virus that would later bear his namesake. Gross injected newborn mice with a slurry of ground-up mouse organs that were known to have leukemia and found that the mice also grew tumors. Later, Stewart and Bernice Eddy of the Biologics Control Laboratory tried the same experiment. Instead of replicating his results, their mice grew tumors of a different kind. “I attempted to confirm his work and instead of getting leukemias, I got tumors of the parotid gland,” Stewart explained, “which were tumors that just had never been observed as spontaneous tumors in mice.”
In 1953, both Stewart and Gross published papers on these induced parotid tumors just months apart. Stewart and Eddy were conservative in their conclusions, maintaining that an “agent” had caused the cancer but avoiding pinpointing it as a cancer-causing virus, which they knew would be controversial. They titled their paper “Leukemia in mice produced by a filterable agent present in AKR leukemic tissues with notes on a sarcoma produced by the same agent.” Both Stewart and Gross insisted that they had discovered the tumors independently, but Gross maintained that he had the results first and therefore deserved credit.
While the debate over proper attribution raged, Stewart kept her eyes on the prize. She knew that to sway the opinion of the scientific community, she would need to establish causation between the agent and the tumors. So she turned to cell culture. First, Stewart isolated tumor extracts that she first cultivated in monkey cells and then in mouse embryos. She and Eddy found that the fluids they harvested from the mouse embryo cultures had higher quantities of the tumor-inducing virus. Their subsequent 1957 paper, “Neoplasms in mice inoculated with tumor agent carried in tissue culture,” concluded that “the most reasonable hypothesis is that it is a virus.” It was the first time a scientist had definitively incriminated a virus as causing cancer.
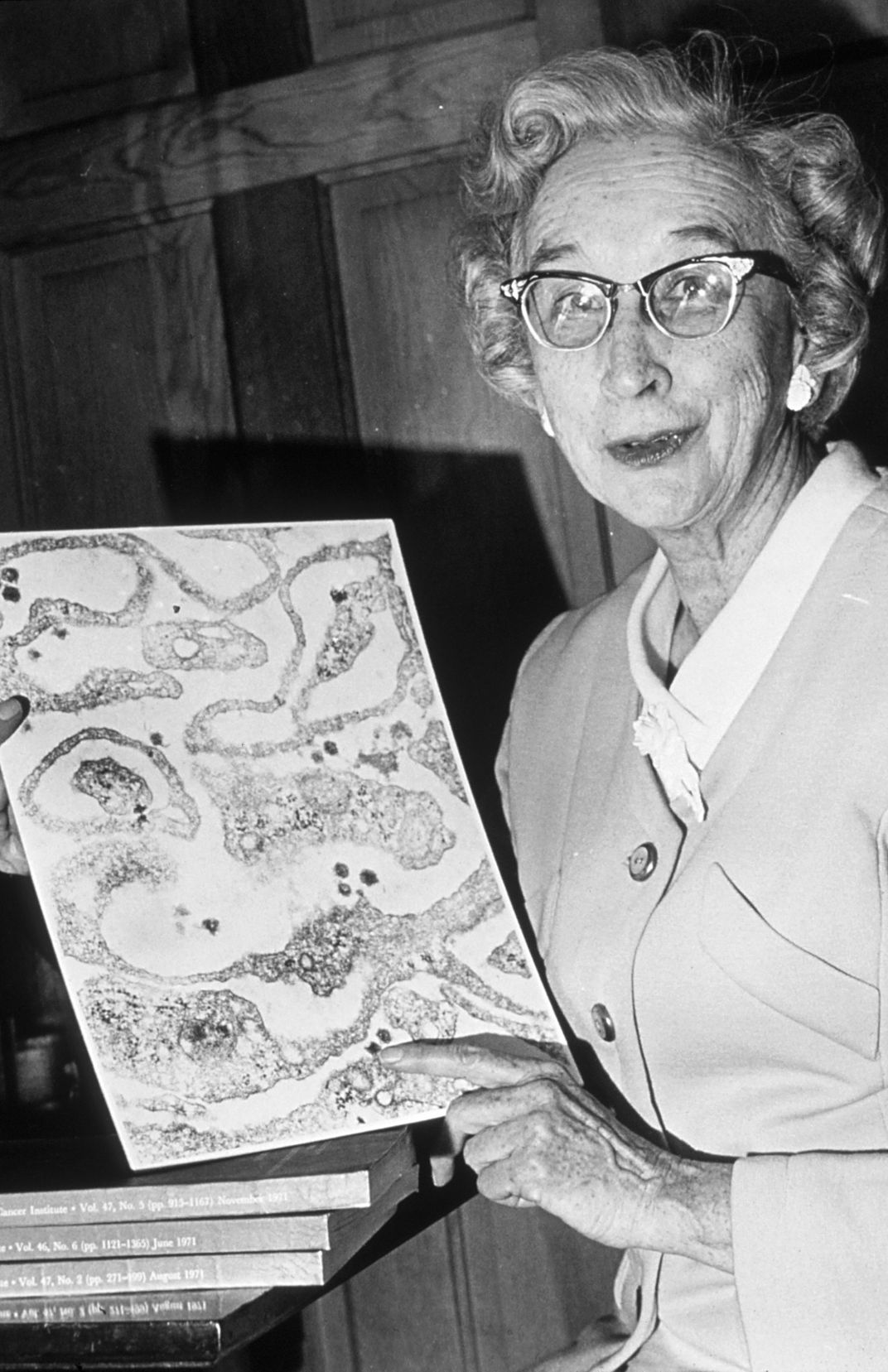
The virus they identified turned out to cause around 20 other kinds of tumors in addition to parotid tumors. So Eddy suggested they call it the polyoma virus, which literally means “many tumors.” In 1958, the pair grew the virus in tissue culture for the first time, and it was named the SE (Stewart-Eddy) polyoma virus in their honor. Elucidating the link between viruses and cancer soon led to a mushrooming of research avenues, leading scientists to better understand the development of both Burkitt’s lymphoma and Hodgkin’s disease. “The whole place just exploded after Sarah found polyoma,” Rabson said. John Heller, then director of NCI, told TIME Magazine that the virus-cancer link was “the hottest thing in cancer research.”
After working on polyoma for 11 years and papilloma for 19, Diana Pastrana, a senior technical laboratory manager at the NIH, says she’s still struck by how effective the virus is on a genetic scale. While human DNA has billions of base pairs to code for all the traits we need to survive, “this virus only has five thousand base pairs to do this with,” she says. “And within that it can do many complex things.” Since the early 2000s, Pastrana says, researchers have been able to discover more and more about polyma’s relationship to human diseases.
Without Stewart and Eddy’s persistence, the HPV vaccine “would never have happened,” Pastrana says. “Thanks to their initial work, a lot of things have been understood. Not only that viruses can cause cancer, but everything that has to do with cancer, like the first genes that they were able to relate to cancer was because of their work.” The pair’s work opened up entirely new avenues of research, including the search for oncogenic viruses in humans. For the rest of her career, Stewart would spend her time hunting down the viruses that contributed to human cancers. In her last paper, published in 1972, she reported on the possible traces of a virus in a human sarcoma.
While applying her scientific knowledge to understanding cancer, Stewart confronted cancer personally. She was first diagnosed with ovarian cancer, and then later with lung cancer, which ended her life in 1976. Eddy, who became Stewart’s long-time friend and colleague, said that Stewart continued her research until she became too ill to work in 1974.
When Stewart entered the field, virus research wasn’t on the National Cancer Institute’s radar. By 1960, the NCI was spending 3.9 million dollars a year investigating the connections Stewart found, according to the Wall Street Journal. Today the NIH boasts a 70 million dollar budget for cancer prevention, which includes research into viruses and cancer. Even though Stewart would not live to see the Gardasil vaccine and other triumphs her work engendered, she did live long enough to see her field move from the fringe of science to the mainstream.