The DNA Data We Have Is Too White. Scientists Want to Fix That
In an era of personalized medicine, not including minorities in genetic studies has real-world health impacts
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/ed/5f/ed5f59a4-e5a4-484e-b671-e31ec53fd08b/screen_shot_2018-04-24_at_41539_pm.png)
We live in the age of big DNA data. Scientists are eagerly sequencing millions of human genomes in the hopes of gleaning information that will revolutionize health care as we know it, from targeted cancer therapies to personalized drugs that will work according to your own genetic makeup.
There’s a big problem, however: the data we have is too white. The vast majority of participants in worldwide genomics research are of European descent. This disparity could potentially leave out minorities from benefitting from the windfall of precision medicine. “It’s hard to tailor treatments for people’s unique needs, if the people who are suffering from those diseases aren’t included in the studies,” explains Jacquelyn Taylor, associate professor in nursing who researches health equity at New York University.
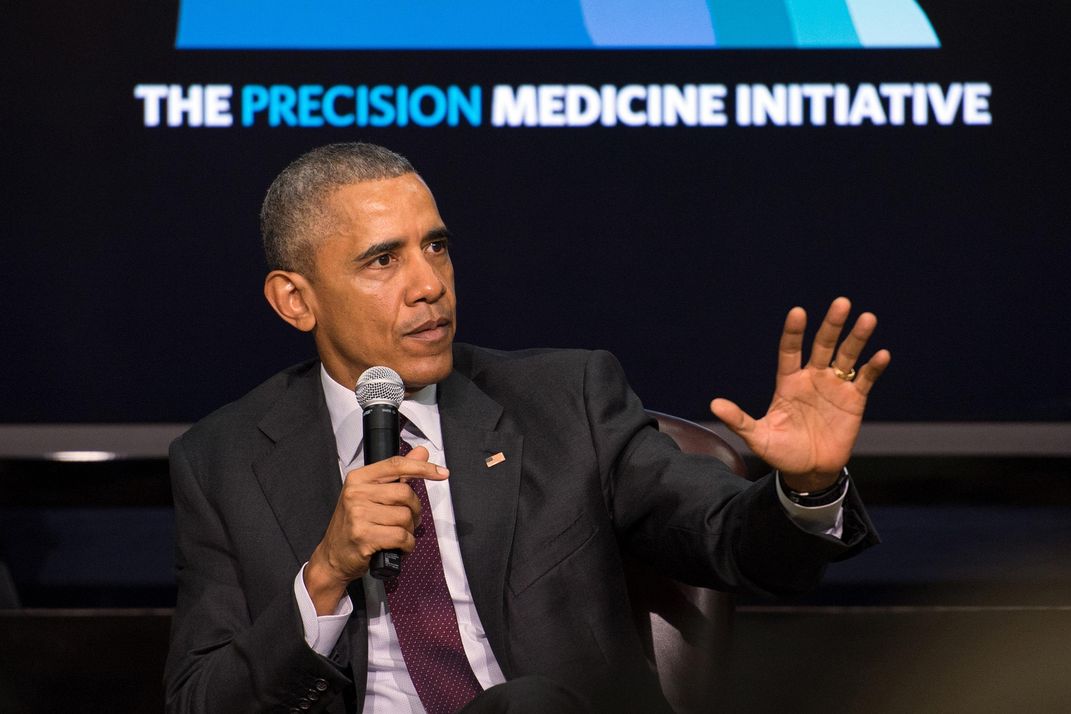
That’s about to change with the “All of Us” initiative, an ambitious health research endeavor by the National Institutes of Health that launches in May. Originally created in 2015 under President Obama as the Precision Medicine Initiative, the project aims to collect data from at least 1 million people of all ages, races, sexual identities, income and education levels. Volunteers will be asked to donate their DNA, complete health surveys and wear fitness and blood pressure trackers to offer clues about the interplay of their stats, their genetics and their environment.
By embracing—and actively seeking out—more minorities in research, the project hopes to give more accurate data about the overall population and fix a long-time discrepancy that has real health impacts. Case in point: African-Americans have the highest prevalence of hypertension of any other group in the United States—about 45 percent, compared to 33 percent on average for whites, says Taylor. “Yet the treatments and standard of care were based on studies of middle-aged white males,” she says.
Currently, there are some 50 large-scale genomics research studies around the world that involve at least 100,000 people, according to remarks by NIH Director Francis Collins at the World Economic Forum in Davos, Switzerland earlier this year. Yet an influential 2016 paper in the journal Nature found that 87 percent of participants in worldwide genomics research were of European descent.
Experts say the lack of diversity is especially alarming in the era of personalized medicine. In order to deliver healthcare recommendations tailored to individuals, researchers need to better understand the biology of your ancestry and ethnicity. If your genetic background isn’t represented in the biobank, you could potentially miss out on certain cures. In other words, you want to make sure they’re using the right answer key to grade your final exam.
“It might be that the Alzheimer’s allele shows up in people of European ancestry, but not as frequently in people of African ancestry or that prostate cancer is unusually aggressive only in people of African descent,” says Eric Topol, director of the Scripps Translational Science Institute and a principal investigator for "All of Us" in San Diego. “But you need to study millions of people to fully understand these associations. The technology is continuing to scale, but that’s not what’s holding us back,” says Topol. “It’s the number and diversity of people.”
In other words, we need more people who are not of European descent.
The 87 percent figure is actually an improvement on the oft-quoted 96 percent statistic from a 2009 article by Duke University data crunchers. But it’s misleading, says Nature co-author Stephanie Fullerton, a bioethicist at the University of Washington. Most of the non-European representation came from national studies in China, Japan and South Korea. Moreover, that increase in diversity didn’t include other minorities. People of African descent only accounted for 3 percent, and Hispanics weighed in at half a percentage point—despite making up 13 percent and 18 percent of the U.S. population, respectively.
In addition to developing individualized cures, researchers are hunting for the holy grail that would revolutionize medicine for the masses: key mutations that could shape the development of future drugs. For example, by studying the genetic makeup of people of African ancestry who had very low cholesterol, researchers found they possessed a mutation that kept their levels low and resulted in fewer heart attacks. The discovery led to the newest class of cholesterol medications known as PCSK9 inhibitors.
“The drug mimics the mutation and is incredibly effective,” says Josh Denny, who specializes in biomedical informatics at Vanderbilt University Medical Center. “By finding the rare population with low cholesterol, researchers were able to identify a drug that might work on all of us.”
Private companies are also aware of the diversity problem. Direct-to consumer genetic sequencing company 23andMe recently received a $1.7 million NIH grant in 2016 to conduct more extensive sequencing of several thousand customers of African-American descent. “Our goal is to build a reference dataset for future health research,” explains project head Adam Auton. “We contacted some of our existing African-American customers to ask them to consent, and more than 80 percent have agreed to participate.”
In an effort to further increase diversity, 23andMe also offers free saliva collection kits to U.S.-based researchers who study underrepresented groups—a project that’s drawn criticism for benefitting mainly American and European commercial interests, reports Sarah Zhang for The Atlantic.

Lingering Mistrust
If minority participation is so highly valued in medical research, why are these communities so noticeably absent from studies?
Experts point to a complex tangle of emotional and practical hurdles. “There’s a history of medical mistreatment that prevents minorities from getting really excited about volunteering,” says Tshaka Cunningham, science advisor for the Minority Coalition for Precision Medicine. Although the story about the use of Henrietta Lacks’ cancer cells without her permission has garnered recent attention, researchers often refer to the enduring legacy of Tuskegee. That’s the government experiment between 1932 and 1972 during which African-American men in Alabama were never told they had syphilis or offered penicillin treatment.
“It’s a fresh psychological scar in the back of many people’s heads,” says Cunningham, also the director of scientific collaboration for Drug Information Association Global. “You can’t help but think, ‘How do I know the same thing won’t happen to me?’ or 'How do I know what they’re going to do with my samples?'”
Similar concerns about lack of consent and privacy provoked the Navajo Nation to outlaw genetic research in 2002, although tribal leaders are currently considering lifting the moratorium to guide the development of new disease treatments.
Minorities might also be shut out of studies because they didn’t have financial or geographic access to the top-level urban medical centers where researchers traditionally have done most of their recruitment, says Fullerton. “If we only study the people who are knocking on our door, we are going to continue to study the same people,” she says.
That’s why All of Us recruiters are trying to knock on other doors—specifically black churches in Baltimore, Bay Area community centers hosting Spanish-language bingo games and nail salons on Chicago’s south side. That’s in addition to establishing partnerships with Walgreens drugstores, Quest Diagnostics labs and local blood banks to expand access for people in remote areas. “There are new players we’ve brought to the table like federally-funded health centers where the most diverse and disenfranchised groups often get access to health care,” says Eric Dishman, director of All of Us. “We’re going to reach the people left behind.” (Dishman is also a personal believer in the power of personalized medicine: He credits genome sequencing with helping him identify a rare form of kidney cancer and received a kidney transplant in time to save his life.)
For many participants in "All of Us," one of the incentives is the chance to learn about their own DNA makeup and future disease risks through genome sequencing, which can cost several hundred to several thousand dollars. But Cunningham of the Minority Coalition for Precision Medicine hopes an altruistic message will hit home for the church congregants he addresses. “I’m a Baptist deacon, so I’m trying to develop the ‘honest broker concept’ by saying, ‘We need to know how our genetics will affect folks like us. We need to know how it will affect your grandbabies,’” he says.
Another strategy that Robert Winn, director of the University of Illinois Cancer Center, is using: Befriending local politicians and business leaders. “Most people overlook the aldermen, but we’re involving them and hoping they send the message to their communities that ‘These guys are good,’” he says. “We’re also hosting presentations in schools and working with minority radio stations. We want to normalize the discussion about genetics.”
Fears About Precision Medicine
The challenge, according to some bioethicists, is that many still hesitate to hand over their genetic data, either to the government or private companies, because they worry it could hurt them later. “For minorities, trust has always been a big issue, but talking about DNA adds a different twist because there are so many nuances about what genetics means,” says Consuelo Wilkins, executive director of the biomedical research alliance between Meharry Medical College and Vanderbilt Medical Center. “People want to make sure their communities don’t miss out on important discoveries, but now the discussion has become ‘What protections are in place?’”
In Stanford bioethicist David Magnus’ focus groups, he learned that minorities viewed donating genetic material more seriously. “Many people believe that DNA samples were a piece of themselves in a way that other health data were not,” he says. “Some people said, ‘What will they do with it? Could they clone another me?’”
Their concerns vary, but a few common ones include the possibility of law enforcement using DNA to falsely accuse people of crimes. While DNA evidence has been instrumental in liberating Death Row inmates, there have also been cases of “false positives” in which innocent people were wrongly implicated in murders. Workplace discrimination is another worry. “One woman asked me, ‘If I’m at high risk for Alzheimer’s, could I lose my job?’” says Wilkins. (For her, a 2008 law that forbids employers or insurance companies from discriminating against you provides little comfort.)
Then there’s the fear that affordable healthcare coverage for people with pre-existing conditions may not be guaranteed—and your genetics can reveal your disease predispositions. “Given the current political environment, people’s fears are not unwarranted,” says Wilkins.
They also questioned whether such research would translate into drugs that would help them or only benefit Big Pharma or insurance companies. “People said, ‘Will this produce medicines we can afford? Or am I helping to create ones that I later won’t be able to afford?'” adds Sandra Soo-Jin Lee, a Stanford anthropologist and bioethicist. “People don’t feel like the research results will serve their best interests.” Some people in the focus groups worried their insurance companies could hypothetically charge them higher copays if their DNA revealed they were part of a group that was found to be susceptible to certain diseases.
“When populations feel vulnerable, the idea of taking on more risk has to be balanced with the idea that there’s value for them, their family or community,” she says.
Dishman says he believes participants understand the value of contributing to a new generation of cures. And he's beginning to see evidence of that hypothesis: After launching the beta phase in May, more than 25,000 people have signed on. The biggest news of all is that more than 70 percent of participants are from underrepresented groups. “We’re really happy with the results so far. We’re hoping to change the game in the long run about who chooses to participate in biomedical research,” he says.
It’s not lost on observers that by embracing science to expose our differences at the most detailed level possible, we may be able to usher in a new era of inclusion. “My hope is that as we get deeper into the study of genomics, we’re going to understand how similar we are as human beings,” says Cunningham. “People will realize we’re less a collection of races. Rather we’re a collection of unique genotypes—each of us beautiful in our own way.”