Why This Robotic Medical Device Belongs in a Museum
William Bargar and Howard “Hap” Paul revolutionized joint replacement surgery by developing a robot to do the job
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/b7/4b/b74b3758-86d6-4d56-aaea-878f05b15db6/istock-613870392.jpg)
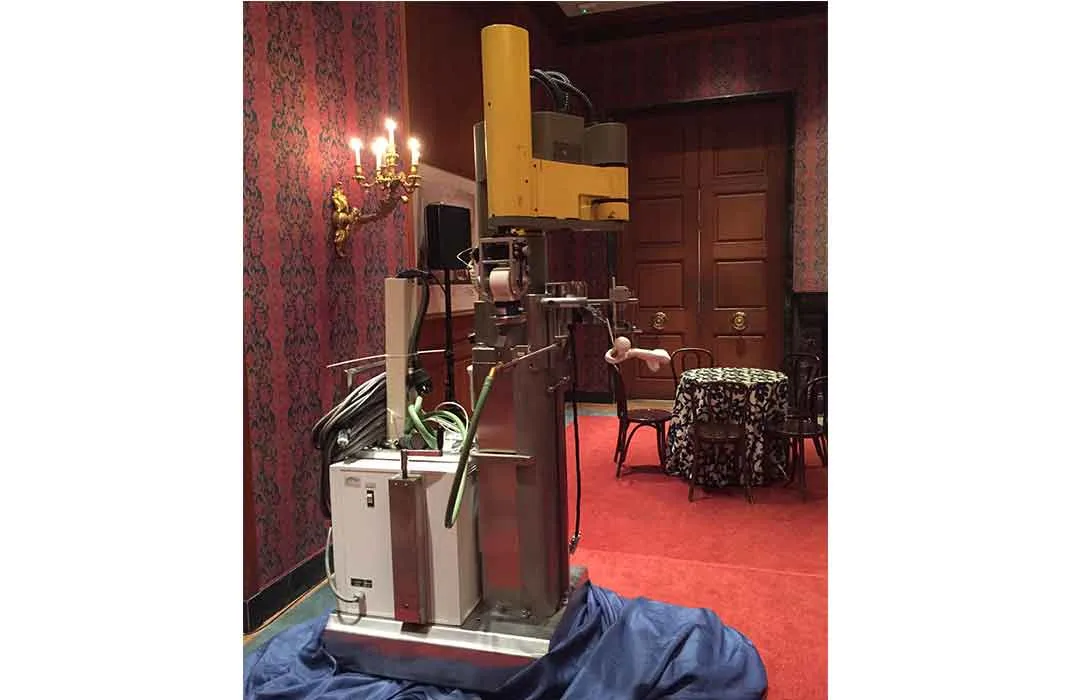
Two and a half years ago, employees at THINK Surgical, a robotic surgery development company in Fremont, California, were cleaning out a storage unit near their headquarters when they found an object that appeared to be an old robot arm.
Upon closer look, Micah Forstein, an assistant manager at the company, realized that the arm was a remnant—a prototype of an invention that had changed joint replacement surgery forever.
Called the Robodoc, the innovative robotic system allows surgeons to perform complicated hip and knee surgeries with greater precision using CT scans converted into three-dimensional virtual images for preoperative planning and computer-guided drilling. The tool has been used in more than 28,000 procedures worldwide.
Now, the fully recovered 1989 prototype will be forever memorialized in the collections of the Smithsonian’s National Museum of American History.
“It’s important for us to remember milestones in medical technology,” says Forstein.
The robot is the brainchild of the late veterinarian Howard "Hap" A. Paul and engineer-turned-orthopedic surgeon William Bargar, who were both working at the University of California, Davis, in the 1980s when Bargar recognized what he calls a dilemma in total hip arthroplasty, or hip replacement surgery.
In that era, implants were attached to the patient’s body with acrylic cement, an impermanent material that would eventually break down, sending the patient back under the knife.
Researchers had already attempted to eliminate the need for the faulty cement by using porous implants in which the bone could actually grow. This development addressed the problem of the deteriorating cement, but the implants were still imperfect because they were only manufactured in a few different sizes; they didn’t fit every patient’s body.
"You’d try to put them in and some would fit too tight," says Bargar, "or you’d break the bone putting it in, or some would fit too loose and it would wiggle, so it was hard to get the right size for every patient. So I had the idea to custom make these things."
Using a patient’s CT scan data along with computer-assisted design/computer-assisted manufacturing (CAD/CAM) technology, Bargar could design an implant to fit a specific individual’s body. He could then transfer the design to a CAD/CAM machine that would cut the implant out of metal.
Meanwhile, on a different part of the UC Davis campus, Paul was studying joint replacement surgeries in dogs as a resident at the School of Veterinary Medicine. He couldn't bear to put a dog down for joint issues if there were alternatives, such as hip replacements. The two researchers joined forces, pursuing custom implant research in dogs.
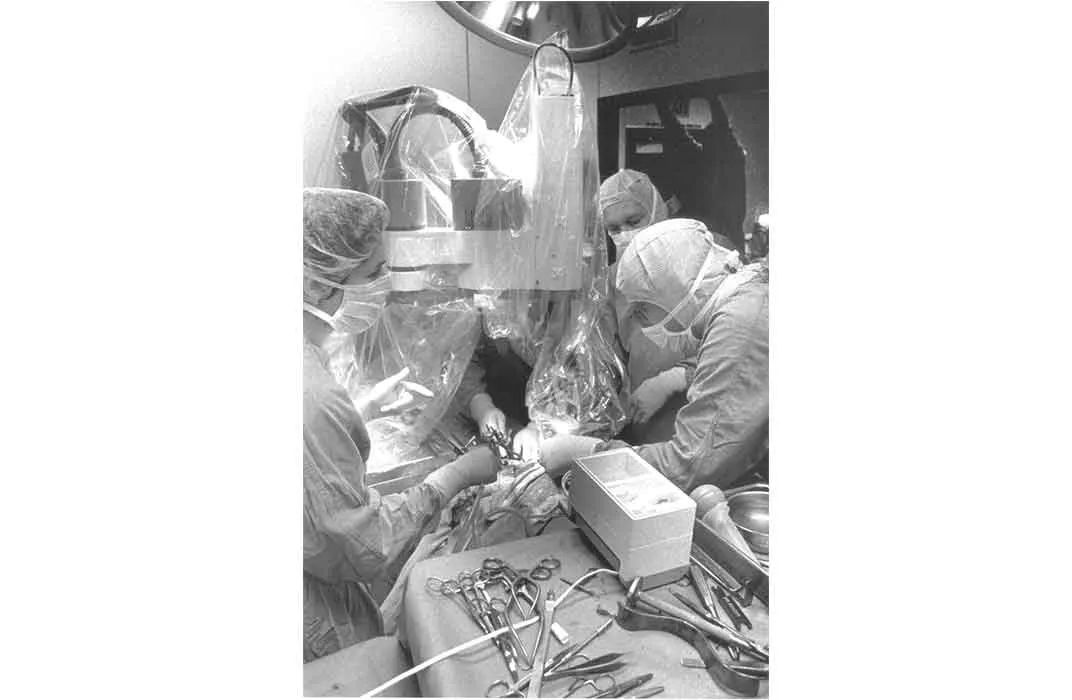
But even with the custom implants, joint replacement surgery was flawed. While a machine made the custom implants, surgeons were still digging the cavities in patients’ bones by hand, often crudely, presenting obstacles for the insertion of the implants and paving the way for harmful consequences, such as bone splintering.
On a flight home from Nice, France, where they had presented their research on the custom implants, Bargar and Paul came up with their next idea: to use a robot to cut the inverse shape of the implant in the patient for a perfect fit.
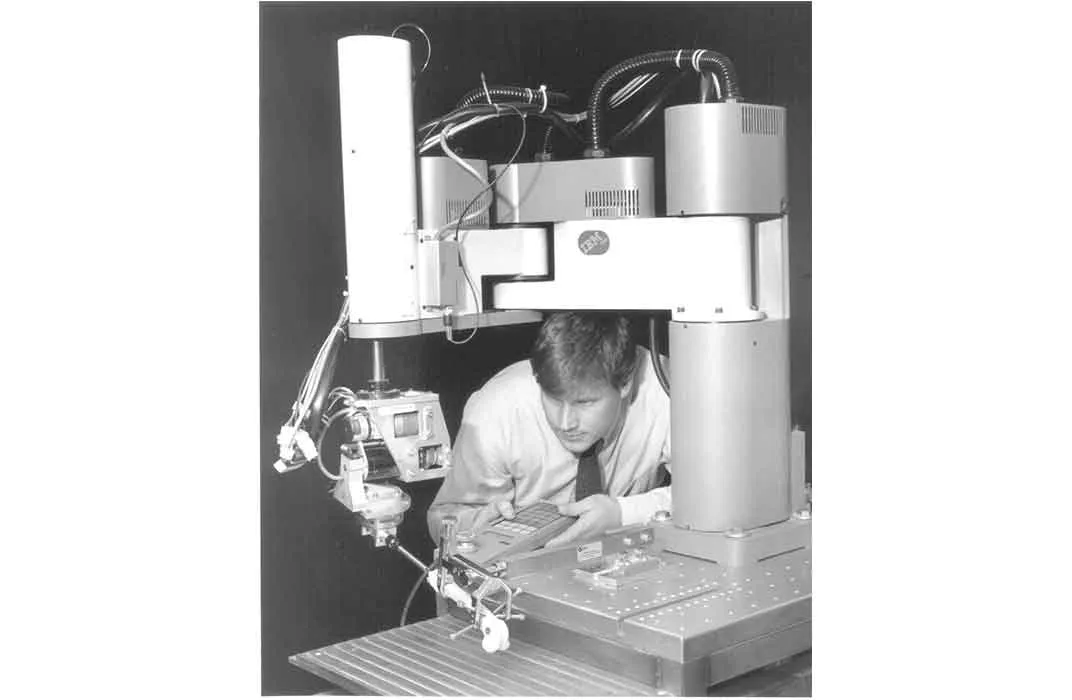
But the research fields of robotics and computers had developed independently of each other, and teaching a robot to act like a CAD/CAM machine was a new concept. After calls to many robotics manufacturers left the researchers at a dead end, Bargar’s father, a former IBM employee, put him in touch with a group at IBM’s Thomas J. Watson Research Lab. There, researchers had developed an automated machine language but had yet to apply it in the real world.
It was the perfect match and in 1986, the researchers began collaborating on the first and only active robotic surgical system. Similarly to the CAD/CAM machine used to manufacture the implants, the robot follows the surgeon’s directions, which it receives from a computer, using this IBM-developed language.
“You have to have an idea and you have to be naive and it also helps to be lucky,” says Bargar.
They christened their robot, Robodoc, in a nod to the popular 1987 film RoboCop. Around 1990, with IBM's support, Paul and Bargar cofounded the company Integrated Surgical Systems and convinced the FDA to allow them to do a feasibility study on a human in November 1992. Between Integrated Surgical Systems and IBM, there are ten patents (numbers 5769092, 5776136, 5806518, 5824085, 6033415, 6322567, 6430434, 5951475, 6415171 and 6747646) that represent different components of the overall invention.
They had already used the robot in surgeries on 23 dogs, and although they had some trouble setting up the machine for the first human surgery, they were successful and proved the safety of the machine.
The FDA then permitted them to complete nine more human surgeries in a multicenter study (Paul participated in six of the test surgeries, but tragically he died of leukemia the day before the final test surgery in the study).
They were able to prove through these studies that the robot aided in more precise joint replacement surgery, but the procedure took longer than a traditional surgery, resulting in greater blood loss. They were able to tweak the process with suggestions from a doctor in Germany who had started using the device around the same time that Bargar’s team began the FDA multicenter studies (the EU had a different set of standards that allowed this device to be used in Europe before it was used in the U.S.).
But to incorporate the changes, the FDA required the team to complete another set of trials, and by 2006, the company was running low on funds. They closed up shop until 2007 when a Korean company called Curexo, the parent company of THINK Surgical, swooped in and provided the funds to complete the study.
The FDA finally cleared the Robodoc the next year, and today, the system is still the only active robotic surgical system (meaning the robot does the procedure itself following the surgeon's commands) used in the U.S. for orthopedic surgery.
Judy Chelnick, an associate curator in the museum’s division of medicine and science, had been following the evolution of robotic surgery technology for years when Forstein made contact with the Smithsonian Institution after uncovering the prototype. Chelnick knew she wanted to collect a robotic medical device, but had yet to decide which one.
After seeing the robot in person in Fremont and researching the Robodoc’s history, she decided this was the most important one to collect first—because it was the first.
“It’s historical. I see it as the evolution of surgery. This is just another way to perform surgery,” says Chelnick.
In November 2016, the National Museum of American History officially inducted the Robodoc into its permanent science and medicine collections. The 72-year-old Bargar, who was present at the dedication ceremony, calls the donation to the Smithsonian a “capper” to his career. “It’s a tremendous honor. It’s probably the biggest accomplishment of my life,” he says.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/DSC_0154.JPG.jpeg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/DSC_0154.JPG.jpeg)