The Unintended (and Deadly) Consequences of Living in the Industrialized World
Scientists believe dirt could explain why some of the wealthiest countries suffer from afflictions rarely seen in less-developed nations
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/The-Secret-Life-of-Dirt-631.jpg)
After eight hours in an overheated Soviet-era sleeper car, we pull into the Petrozavodsk train station just after 1 a.m. The streets are silent, the night air chilly. Our taxi shudders and swerves along roads pitted with axle-gulping potholes. Identical concrete apartment blocks built in the 1960s flash by in a blur. Winter temperatures here, some 250 miles northeast of St. Petersburg, sometimes plunge to minus 40 degrees Fahrenheit. A traffic circle in the middle of town boasts what locals claim is Russia’s only statue of Lenin holding a fur hat.
I’m traveling with Mikael Knip, a short, energetic Finnish physician and University of Helsinki researcher with a perpetual smile under his bushy mustache. He has come to Petrozavodsk—an impoverished Russian city of 270,000 on the shores of Lake Onega and the capital of the Republic of Karelia—to solve a medical mystery, and perhaps help explain a scourge increasingly afflicting the developed world, the United States included.
For reasons that no one has been able to identify, Finland has the world’s highest rate of Type 1 diabetes among children. Out of every 100,000 Finnish kids, 64 are diagnosed annually with the disease, in which the body’s immune system declares war on the cells that produce insulin. Type 1 diabetes is usually diagnosed in children, adolescents and young adults.
The disease rate wasn’t always so high. In the 1950s, Finland had less than a quarter of the Type 1 diabetes it has today. Over the past half-century, much of the industrialized world has also seen a proliferation of the once rare disease, along with other autoimmune disorders such as rheumatoid arthritis and celiac disease. Meanwhile, such afflictions remain relatively rare in poorer, less-developed nations.
Why?
Petrozavodsk, only about 175 miles from the Finland border, may be the perfect place to investigate the question: The rate of childhood Type 1 diabetes in Russian Karelia is one-sixth that of Finland. That stark difference intrigues Knip and others because the two populations for the most part are genetically similar, even sharing risk factors for Type 1 diabetes. They also live in the same subarctic environment of pine forests and pristine lakes, dark, bitter winters and long summer days. Still, the 500-mile boundary between Finland and this Russian republic marks one of the steepest standard-of-living gradients in the world: Finns are seven times richer than their neighbors across the border. “The difference is even greater than between Mexico and the U.S.,” Knip tells me.
Since 2008, Knip and his colleagues have collected tens of thousands of tissue samples from babies and young children in Russia and Finland, as well as in nearby Estonia. In his spotless lab on the fourth floor of a modern research complex in Helsinki, nearly two dozen freezers are filled with bar-coded vials of, among other things, umbilical cord blood, stool samples and nasal swabs. The freezers also hold tap water and dust collected at the different locations. By comparing the samples, Knip hopes to isolate what’s driving Finland’s diabetes rate up—or what’s keeping Russian Karelia’s low.
For all the sophisticated analysis involved, the theory that Knip is testing couldn’t be more basic. He thinks the key difference between the two populations is...dirt. In a sense, he wonders if kids in Finland, and in the United States and other developed nations as well, are too clean for their own good.
***
The idea that dirt, or the lack of it, might play a role in autoimmune disease and allergy gained support along another border. In the late 1980s, Erika von Mutius was studying asthma in and around Munich. At the time, researchers thought air pollution was the cause. But after years of work, the young German researcher couldn’t clearly link Munich’s pollution and respiratory disease.
On November 9, 1989, an unusual opportunity came along: The Berlin Wall fell. For the first time since the 1940s, West Germans could conduct research in the East. Von Mutius, of Ludwig-Maximilians University Munich, seized the opportunity, expanding her study to include Leipzig, a city of 520,000 deep in East Germany.
The countryside around Leipzig was home to polluting chemical plants and was pocked with open-pit coal mines; many residents heated their apartments with coal-burning ovens. It was a perfect experiment: Two groups of children with similar genetic backgrounds, divided by the Iron Curtain into dramatically different environments. If air pollution caused asthma, Leipzig’s kids should be off the charts.
Working with local doctors, von Mutius studied hundreds of East German schoolchildren. “The results were a complete surprise,” von Mutius says. “In fact, at first we thought we should re-enter the data.” Young Leipzigers had slightly lower rates of asthma than their Bavarian counterparts—and dramatically less hay fever, a pollen allergy.
Puzzling over her results, von Mutius came across a paper by David Strachan, a British physician who had examined the medical records of 17,000 British children for clues to what caused allergies later in life. Strachan found that kids with a lot of older brothers and sisters had lower rates of hay fever and eczema, probably because the siblings brought home colds, flus and other germs.
After learning of Strachan’s study, von Mutius wondered whether air pollution might somehow protect East Germans from respiratory allergies.
Soon, studies from around the world showed similarly surprising results. But it was germ-laden dirt that seemed to matter, not air pollution. The children of full-time farmers in rural Switzerland and Bavaria, for example, had far fewer allergies than their non-farming peers. And a study following more than 1,000 babies in Arizona showed that, unless parents also had asthma, living in houses with dogs reduced the chances of wheezing and allergies later in life. Researchers proposed that the more microbial agents that children are exposed to early in life, the less likely they are to develop allergies and autoimmune diseases later on. Studies also showed that baby mice kept in sterile environments were more likely to face autoimmune disease, seeming to back what came to be called the “hygiene hypothesis.”
“It was so unexpected,” says von Mutius, who now believes air pollution was a red herring. Instead, East German children may have benefited from time spent in daycare.
Think about it this way: At birth, our immune cells make up an aggressive army with no sense of who its enemies are. But the more bad guys the immune system is exposed to during life’s early years, the more discerning it gets. “The immune system is programmed within the first two years of life,” says Knip. “With less early infection, the immune system has too little to do, so it starts looking for other targets.”
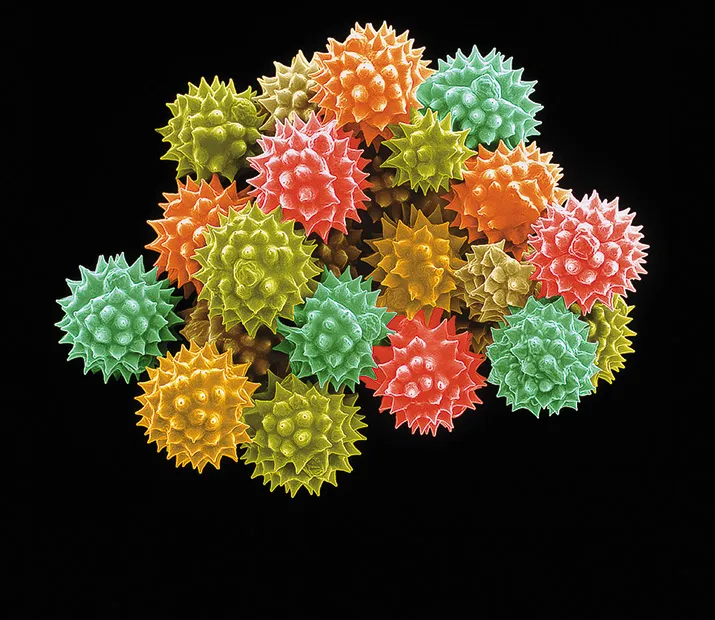
Sometimes the immune system overreacts to things it should simply ignore, like cat dander, eggs, peanuts or pollen. Those are allergies. And sometimes the immune system turns on the body itself, attacking the cells we need to produce insulin (Type 1 diabetes) or hair follicles (alopecia) or even targeting the central nervous system (multiple sclerosis). Those are autoimmune disorders.
Both appear to be mostly modern phenomena. A century ago, more people lived on farms or in the countryside. Antibiotics hadn’t been invented yet. Families were larger, and children spent more time outside. Water came straight from wells, lakes and rivers. Kids running barefoot picked up parasites like hookworms. All these circumstances gave young immune systems a workout, keeping allergy and autoimmune diseases at bay.
In places where living conditions resemble this “pre-hygiene” past—rural parts of Africa, South America and Asia—the disorders remain uncommon. It can be tempting to dismiss the differences as genetic. But disease rates in the industrialized world have risen too fast, up to 3 or 4 percent a year in recent decades, to be explained by evolutionary changes in DNA. “You can see quite clearly in a pre-hygiene situation you don’t see allergic disease,” says Thomas Platts-Mills, an allergy specialist at the University of Virginia. “Move to a hygiene society, and it does not matter your race or ethnicity—allergy rises.”
These findings don’t mean that people should eschew basic hygiene. Its benefits are clear: In the past 60 years or so, our overall life expectancy has continued to rise. The trick for scientists is to determine exactly which early life exposures to germs might matter and identify the biology behind their potentially protective effect.
That’s one big way Knip’s research on the Finland-Russia border can contribute. The accident of geography and history playing out there offers a chance to work in what Knip calls a “living laboratory.”
“It’s really an exciting opportunity,” says Richard Insel, chief scientific officer for the New York City-based Juvenile Diabetes Research Foundation.
***
Just a few hours after we arrive in Petrozavodsk, I follow Knip and his team to a morning meeting at the Karelian Ministry of Health. Russian officials on the other side of a long conference table explain through an interpreter that they haven’t recruited as many study participants as their Finnish and Estonian colleagues. Parents in Petrozavodsk are unfamiliar with the practice of conducting medical studies, reluctant to submit their babies to what they see as painful blood tests and too stressed to fill out long surveys on diet and family history.
If Knip is frustrated, he hides it well. The recruitment phase of the study was supposed to end in 2012. He’s trying to buy his Russian colleagues another year to conduct their work, he says, smiling and shaking hands before heading to a taxi waiting outside. “It’s turned out to be a lot more complicated than we expected,” Knip tells me later. “Cultural differences have been a big learning process for us.”
The next stop is Petrozavodsk Children’s Hospital, a building on the city’s outskirts surrounded by concrete apartments. While Knip gives a pep talk to pediatricians charged with gathering study samples, I sit down with Tatyana Varlamova, a young doctor in a thigh-length white lab coat and black pumps. Varlamova’s drab exam room is a world away from Knip’s gleaming lab in Helsinki. It’s equipped with a plug-in space heater and particleboard desk. Wilted potted plants sit next to an open window. In a long corridor outside are wood benches filled with exhausted-looking parents and children edging toward tears.
Varlamova is clear-eyed about the differences between Russian Karelia and Finland. “Karelia is poorer,” she says, “there’s no hysterical cleaning of apartments and a lot more physical activity.”
Conducting the study in Russia has been a struggle, she says. While extra attention from doctors encourages Finnish and Estonian parents to participate, that’s not the case in Russia. Babies here are already required to visit a pediatrician once a month in the first year of life, more often than in Finland. Enrolling young children has also been challenging. Since 2008, doctors have seen 1,575 children in Espoo, a suburb of Helsinki; 1,681 have been sampled in Estonia, where the diabetes rate falls between that of Finland and of Russian Karelia. But after three years, researchers had recruited only 320 Russian children.
“People don’t need more time with the doctor,” Varlamova tells me softly in Russian. “They’re not as motivated to take part in scientific investigations. They have more important problems in their life.”
Then there’s the Russian bureaucracy. All the samples taken for the study have to be analyzed in the same Finnish lab for consistency. But just as Knip’s study was taking shape, Russian legislators passed a law requiring special permission to export human tissue samples. (Some lawmakers argued that foreigners might use the samples to develop biological weapons targeting Russians.) As a result, Varlamova explains, thousands of study samples from Petrozavodsk had to be individually reviewed by three ministries, including the dauntingly named Federal Agency for the Legal Protection of Military, Special and Dual-Use Intellectual Property, before being exported. Finally, though, samples going all the way back to 2008 and filling two industrial freezers crossed the border into Finland last December, along with a 30-pound stack of paperwork.
Early results are pointing to different immune system challenges during infancy in the study regions. Russian children, Knip says, spend the first years of their lives fighting off a host of infections virtually unknown in Finland. The Russian kids, as other studies have shown, have signs of regular exposure to hepatitis A, the parasite Toxoplasma gondii and the stomach bug Helicobacter pylori. “Helicobacter pylori antibodies are 15 times more common in children in Russian Karelia than in Finland,” says Knip. “We did expect more microbial infections. But we didn’t expect such a huge difference.”
Identifying important differences may lead to a Type 1 diabetes prevention strategy, for kids in Finland and the rest of the developed world. “If one could identify specific microbes, you’d have to consider whether you could expose children—in a safe way—to those microbes,” Knip says.
Such an intervention could prime the immune system much like a vaccine, but might use a collection of bacteria rather than a specific microbe.
Knip’s in a hurry to find out: Living laboratories don’t last forever.
Von Mutius, for her part, says she might have missed her chance to prove her hypothesis that crowded daycare centers, not pollution, protected kids in East Germany. Leipzig’s coal pits have been flooded and turned into lakes ringed with beaches and bike paths. “We cannot go back—the East and West German phenomenon will remain an enigma,” von Mutius says.
In Russia, Karelia’s living standards, though they lag behind those in the most developed nations, have been rising slowly—alongside cases of Type 1 diabetes, celiac disease, hay fever and asthma.
If Knip and his team can identify the culprits soon enough, perhaps Karelia, and other developing regions, can enjoy the upsides of modernity without some of the disorders that have accompanied economic advancement elsewhere in the world.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/SQJ_1604_Danube_Contribs_02.jpg)

/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/SQJ_1604_Danube_Contribs_02.jpg)