Help for the Brokenhearted: Wearable, Biosynthetic and ‘Beatless’ Artificial Hearts
Cow-machine hybrids and continuous-flow technologies are helping people survive devastating heart failure
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/c3/d3/c3d3d050-f8f0-41a0-80bf-75f0bb7899d8/42-34662110.jpg)
Jilted valentines may say there's no cure for a broken heart. But help is on the way for those whose actual hearts are ailing, thanks to an innovative suite of technologies that could one day benefit the millions of people suffering from heart failure.
The heart uses four chambers to pump blood throughout the body: one atrium and one ventricle on each side. After blood is enriched with oxygen in the lungs, it's sent into the left atrium and through the left ventricle so it can be pumped throughout the body. Oxygen-depleted blood returns to the heart's right atrium, then moves to the right ventricle and is pumped back into the lungs.
Most heart transplant patients have been hospitalized multiple times for severe heart failure because one or both sides of their hearts don't function properly. That's commonly caused by damage to heart muscles or the chambers' valves, coronary heart disease, hereditary conditions or viral infections.
“Wearable” Heart Machines

Only 2,000 to 2,500 donor hearts become available each year in the U.S., which means that thousands of critically ill patients must wait months or even years for a transplant—if they can survive that long. The SynCardia Total Artificial Heart, heir to technology used in the famed Jarvik devices of the 1980s, is by far the most commonly used artificial heart, with more than 1,350 successful implants since it was approved for use. It acts as a critical bridge, enabling patients suffering from biventricular end-stage heart failure to survive until a human transplant becomes available.
Until recently, though, many people using the SynCardia device were confined to the hospital, because the heart's motors and electronics are housed outside the body in a large, heavy driver device. The driver connects to the artificial heart with two tubes, and it creates an artificial heartbeat by filling “balloons” inside the device's artificial ventricles. That pushes blood out into the circulatory system at a rate of 2.5 gallons per minute. The system simplifies the moving parts inside the artificial heart itself, which accounts, in part, for its extremely low failure rate of less than one percent.
But the reduced quality of life for patients stuck in a hospital room can take its toll. So after four years of tests, the FDA approved the Freedom portable driver in July 2014. In use in Europe since 2010, this device enables patients to replace the dishwasher-sized hospital drivers with a smaller unit that weighs just 13.5 pounds. It can be carried in a backpack or wheeled in a rolling caddy or walker. The unit runs on lithium-ion batteries and can be recharged by plugging into a standard wall outlet or car charger, allowing patients to return home and live relatively normal lives while awaiting transplants.
How much can the device help an artificial heart recipient? Consider the case of Randy Shepherd: As a teenager, his heart had been damaged by rheumatic fever and its two ventricles could no longer pump enough blood to keep him alive. Shepherd received a SynCardia heart in June 2013. Less than a year later, Shepherd used his Freedom unit to complete a 4.2-mile walk as an entrant in Pat's Run near Phoenix, Arizona.
“While I don’t necessarily feel inspirational, I do feel [that] showing people what is possible is important, that life doesn’t end with a bad medical diagnosis,” he wrote soon after the event in a Reddit Ask Me Anything. Shepherd, known as the "Tin Man,” received a donor heart transplant in October 2014 after living with his artificial heart for 15 months. He speculates that the physical activity he was able to enjoy with the Freedom unit may have even increased his odds of a successful recovery.
Part Machine, Part Cow
For most patients, a SynCardia heart is meant to be a stopgap until a donor heat is available. The more challenging goal is to design a permanent solution.
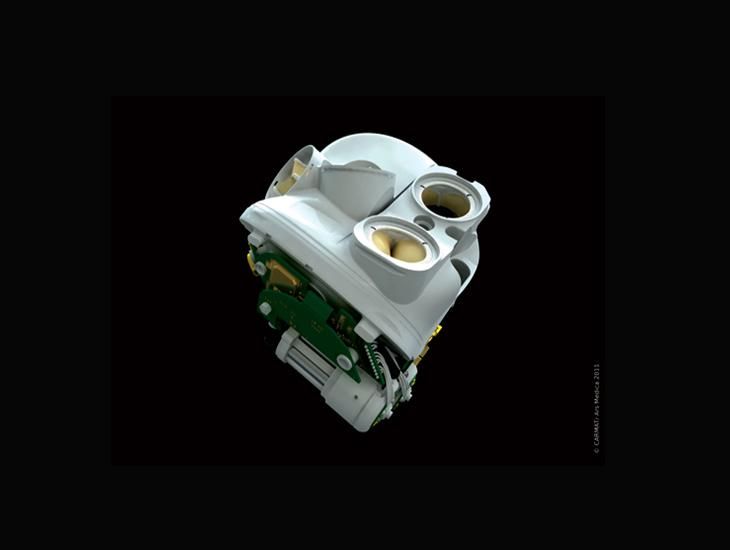
In France, researchers are using a mix of artificial and biological components to do just that. The CARMAT artificial heart is made of two chambers divided in half by a membrane. One side is home to a pumping system of motors and fluids, which move the membrane to force blood from the other side out into the circulatory system. Sensors and microelectronic controls monitor pressure and adjust flow rates to match a patient's activity—allowing the heart rate to accommodate exercise, for example.
The membrane surface facing the pumping system is made of polyurethane, while the flip side in contact with human blood has been constructed of tissues from cow hearts. The heart's artificial valves are also made of cow tissue, and designers hope that these chemically sterilized biological materials will alleviate problems that have plagued past artificial hearts. For instance, the body's incompatibility with synthetic materials can destroy red blood cells or trigger clotting.
The CARMAT heart's first recipient, a terminally ill 76-year-old man, received the implant in December 2013 and died in March of the following year. The second patient to be fitted with the device left Nantes University Hospital on January 19 armed with a light, portable external battery supply. The man received the heart last summer as part of a clinical trial.
“Our greatest reward has been the patient’s joy at not only reclaiming a level of activity that was unthinkable just a few months ago thanks to the bioprosthesis, but more importantly being able to live a real life at home with family and friends,” CARMAT chief executive officer Marcello Conviti said in a press statement.
Living Without a Heartbeat
In addition to risks from biological rejection, a big problem for artificial heart designers has been matching the incredible durability of Mother Nature's design. A healthy human heart has to pump some 35 million times a year, an incredible workload that engineers have had a hard time accommodating with any device.
Researchers at the Texas Heart Institute are tackling that problem with an end run around the issue—creating a heart that doesn't beat at all, but instead provides a continual flow of blood. Their BiVACOR total artificial heart concept has some proven history behind it. When both sides of a heart are failing, a transplant becomes necessary. But if only one side isn't pumping properly, the heart may be treated with flow-boosting implants. Left Ventricular Assist Devices (LVADs) are continuous-flow implants that boost ailing hearts with a constantly spinning impeller that pushes blood through the body—sometimes taking over most or nearly all of the human heart's pumping output. More than 20,000 people currently sport these turbine-like heart helpers.
Seeking to expand this technology to whole-heart replacement, researchers have designed a device with just one moving part: a rotor with two blades that spins within a small titanium chamber. A smaller blade forces blood through the right chamber to the lungs, while a larger one moves it out of the left chamber to the circulatory system and through the body. The rotor is suspended by magnetic fields, which further reduces wear by eliminating friction. MAGLEV technology controls the rotation of the blades to match the user's activity level.
The BiVACOR heart is one of the few options small enough to be implanted in a child, a key advance over other artificial efforts that can be too bulky even for smaller adults. Like all artificial heart technologies to date, the system has potential downsides. Replacing the natural pumping with a propeller subjects the blood to a bit of frothing that may promote internal bleeding, strokes or other complications. But the concept has at least one early success story.
A previous version of BiVACOR was implanted in a terminally ill patient, Craig Lewis, at the Texas Heart Institute in March 2011. Lewis lived for six weeks before dying of liver and kidney failure related to his heart condition, which was so dire that no current treatment would have delivered a longer lifespan. But he proved that it was possible to survive for longer than thought possible with just the gentle whirring noise of a propeller inside his chest.