Doctors’ Stethoscopes Can Transmit Bacteria As Easily As Unwashed Hands
New research shows that the instruments could be a vector for bacterial infections—a concern, as they’re infrequently sterilized
:focal(742x957:743x958)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/32/07/32076f55-ea66-4853-a57f-fa09212a329c/stethoscope.jpg)
In recent years, it's become painfully clear to everyone working in medicine that frequent hand washing is crucial to stopping the spread of infection in hospital settings. Nowadays, every hospital and clinic posts signs that remind doctors and other health professionals to clean or sterilize their hands in between seeing every patient.
Doctors' hands, though, aren't the only things that come into contact with sick patients over and over again. The trusty stethoscope, one of the most basic and important tools in a physician's kit, can touch dozens of patients during a day and is sanitized much less often than a pair of hands—potentially raising the risk for cross-transmission of harmful bacteria and other microbes between patients.
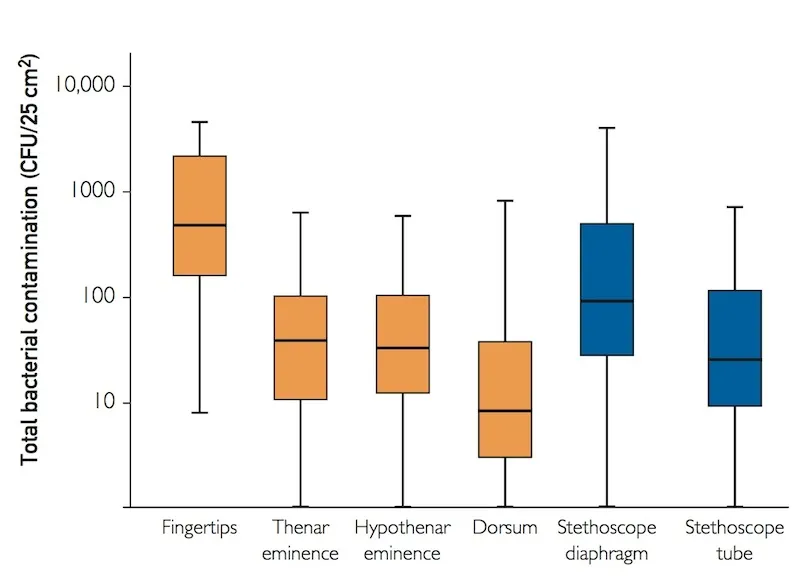
To prove this point, Didier Pittet and colleagues at the University of Geneva Hospitals—a team that has been conducting research into hand hygiene for more than two decades—directly compared the amount of bacterial contamination on a doctor's hands and a previously-sterilized stethoscope after each time the doctor examined a patient. As they report today in Mayo Clinic Proceedings, the stethoscopes' diaphragms (the circular part that comes into contact with the patient's skin) were, on average, much more contaminated than most parts of the gloves on doctors' hands, second only to their fingertips, which are known to carry the highest concentrations of bacteria.
Of course, if a doctor does what the researchers did, and sterilizes the stethoscope with an alcohol-based sanitizer or other method after seeing each patient, this wouldn't be such a problem. But Pittet believes that's seldom the case, and the data back him up.
"Physicians forget to clean their hands quite frequently, even in the best places," he says. "When they forget to clean their hands, they certainly forget to disinfect their stethoscope. And from my experience, even those who are really good models of hand hygiene likely forget to clean their stethoscopes most of the time."
Previous work had looked at contamination on stethoscopes in isolation, but as the researchers note, pretty much all surfaces in hospital rooms (and in the real world) harbor bacteria. To see if stethoscopes are actually a relevant threat in spreading infection, they'd have to be rigorously compared to doctors' hands, which are known to be a vector for harmful bacteria if not properly cleaned.
To make this comparison, Pittet's team asked three different doctors to conduct a standard examination of a total of 33 different hospitalized patients, sterilizing their stethoscopes and putting on sterile gloves beforehand each time. After each exam, they cultured the bacteria they found on two parts of the stethoscopes (the tube and diaphragm) and four different areas of the gloves on doctors' dominant hands (fingertips, back of hand, and either side of the palm).
The cultures revealed that, while the doctors' fingertips had the highest concentrations of bacteria, the diaphragms of their stethoscopes had the second-most, far more than their palms or the back of their hands. There was a strong correlation between exams that produced contaminated fingertips and contaminated stethoscopes, suggesting that both surfaces were equally likely to pick up bacteria up from patients.
In a separate phase, the researchers had doctors conduct examinations bare-handed with 50 other hospital patients, and after each exam, they tested for MRSA—methicillin-resistant Staphylococcus aureus, a strain of bacteria that's impervious to several classes of antibiotics and a medical concern because of how difficult its infections can be to treat.
This type of bacteria was found on the doctors' hands after 38 of the 50 exams, but whenever it was, it was detected in substantial concentrations on the stethoscope diaphragms as well, in numbers much higher than the back and palms of the doctors' hands and nearly as high as the doctors' fingertips. In some cases, even the stethoscope tubes had picked up MRSA, likely from the physicians' own hands, as they held the tubes after touching the patients.
Next, Pittet plans go a step further, testing not only how often stethoscopes become contaminated after a doctor sees a patient, but how likely it is that an unsterilized stethoscope can pass that bacteria on to the next one.
He also plans to work on something more mundane: a better stethoscope cleaner. Although some doctors simply don't remember to clean their stethoscopes, others, Pittet says, may be reluctant to damage them with the alcohol-based sanitizers or wipes found to be effective in sterilizing the instruments.
"If I showed you my old stethoscope, which I used for more than 30 years, and that I cleaned with an alcohol-based cleanser after each patient, you can see that the plastic [tubing] has been highly damaged," he says. "It's not a big deal—it's a $13 cost for 30 years of practice—but nevertheless, it tells you that it's not easy to clean your stethoscope as often as needed."
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/joseph-stromberg-240.jpg)
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/joseph-stromberg-240.jpg)